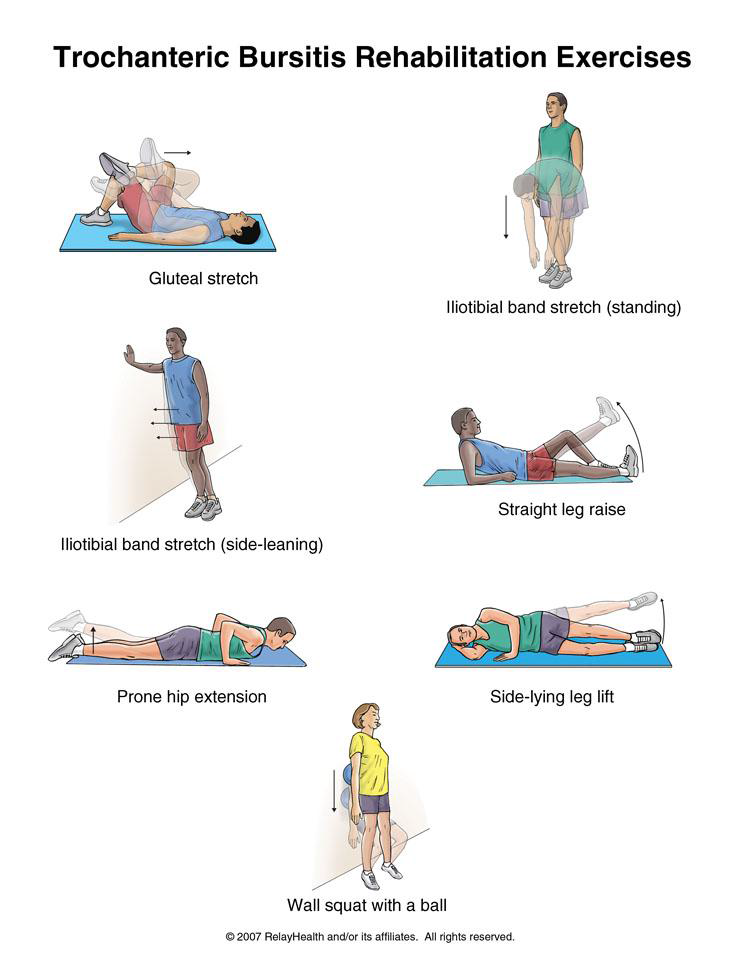
You can begin stretching the muscles that run along the outside of your hip using the first 3 exercises. You can do the strengthening exercises when the sharp pain lessens.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
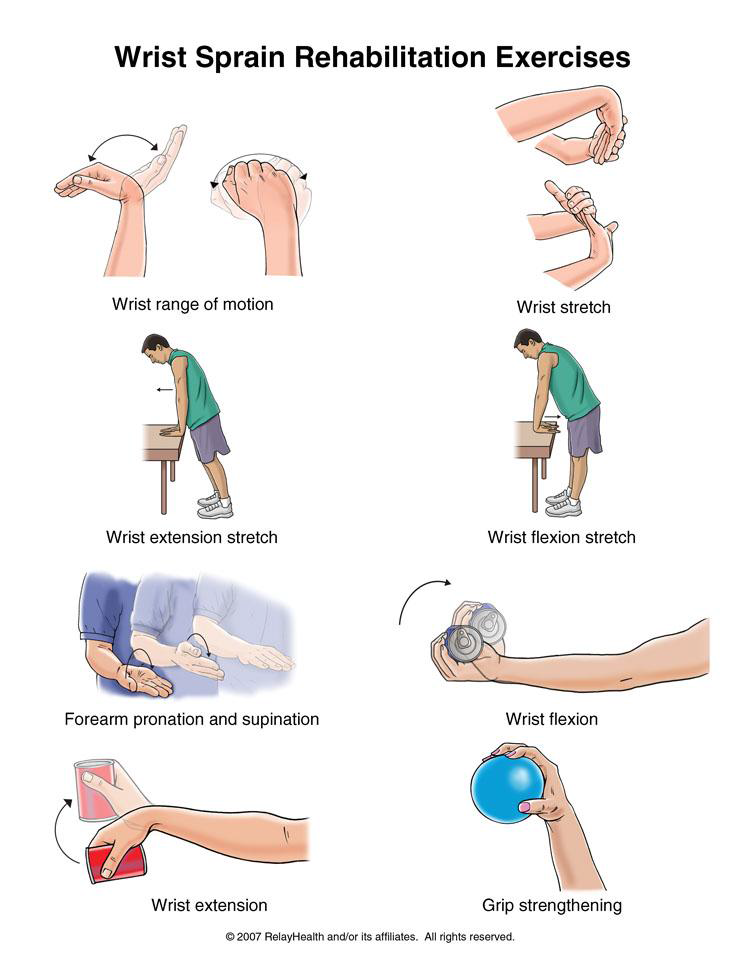
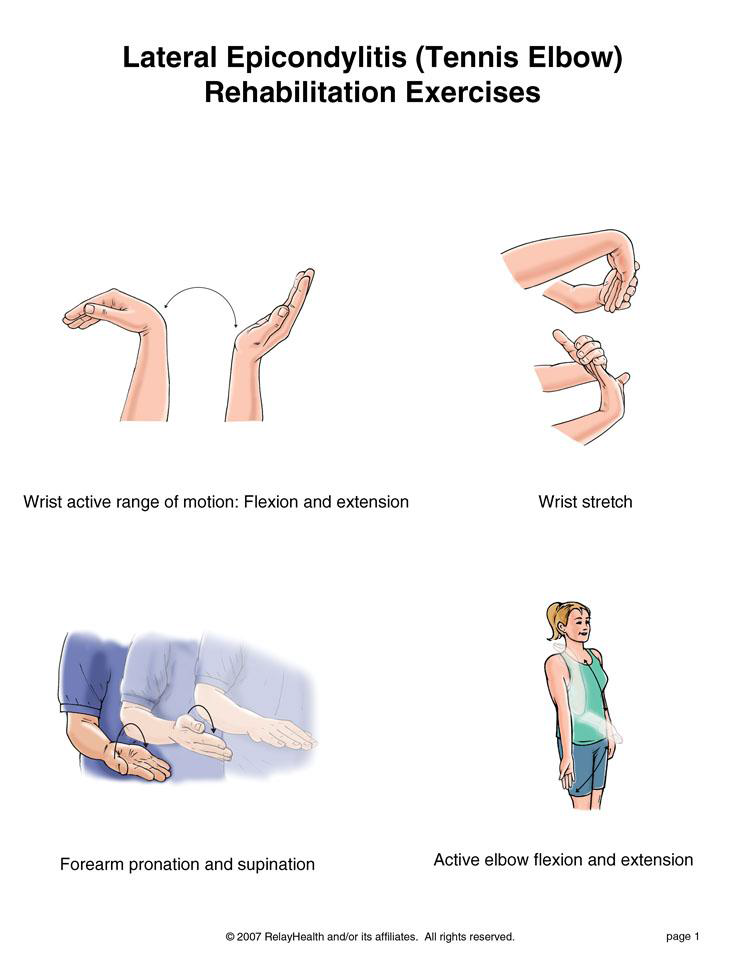
The first 5 exercises are stretching exercises. You may do these when the sharp wrist pain goes away. The last 3 exercises are strengthening exercises. You may do these exercises when stretching is nearly painless.
When this exercise becomes pain free, do it with some weight in your hand such as a soup can or hammer handle.
starting position. Do 3 sets of 10. Gradually increase the weight of the object you are holding.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
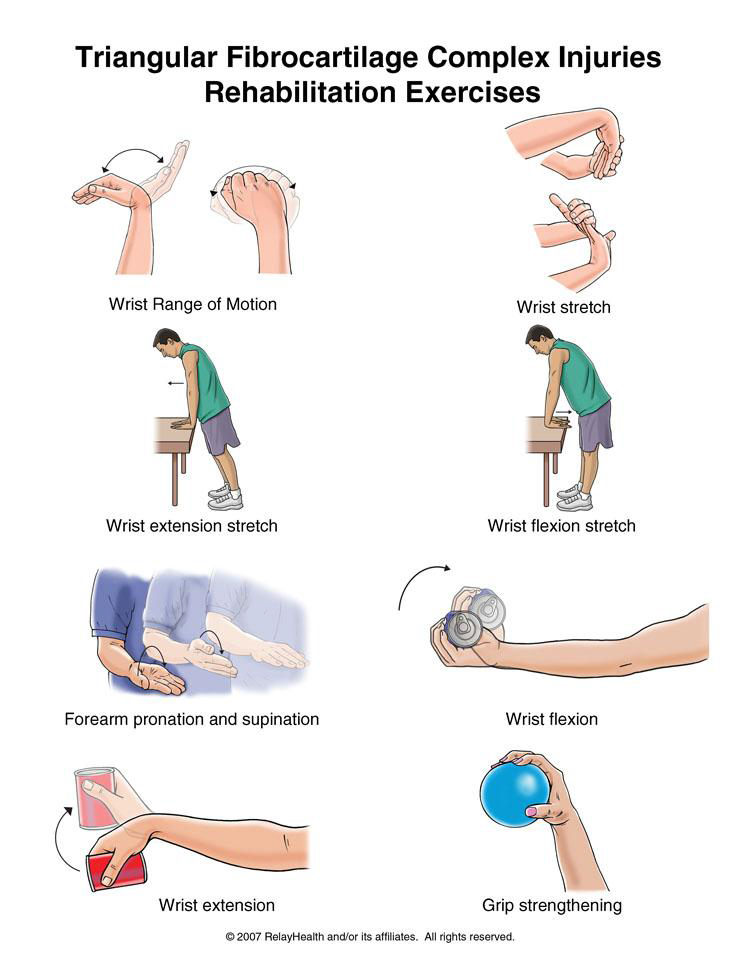
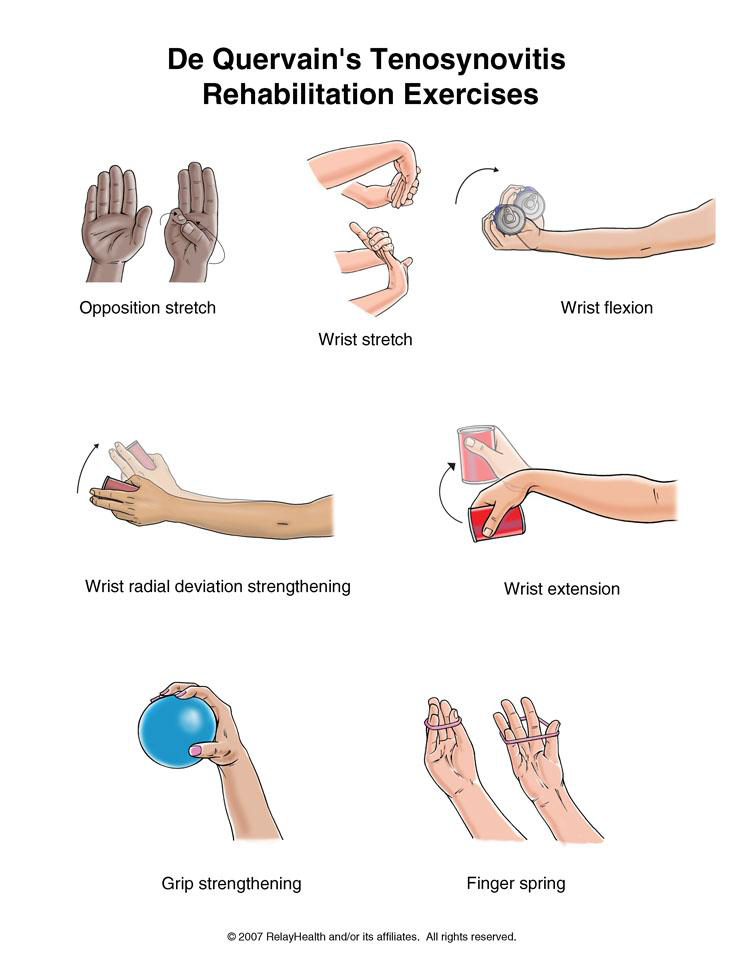
You may do the stretching exercises when the sharp wrist pain goes away. You may do the strengthening exercises when stretching is nearly painless.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
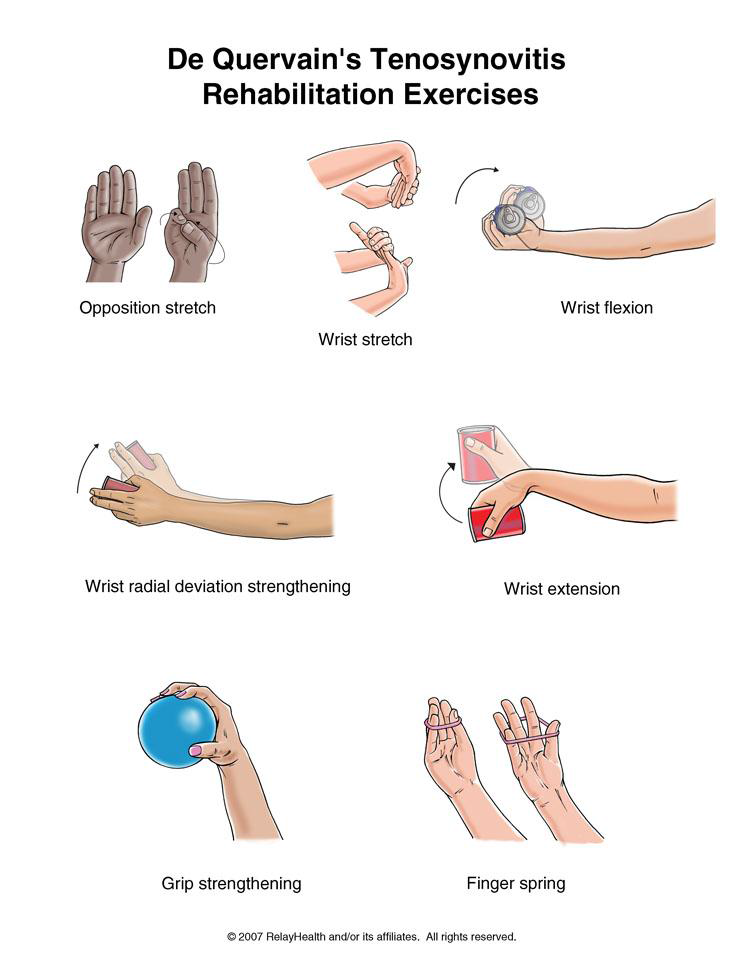
You may do all of these exercises when the initial pain is gone.
Written by Scott Coleman, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
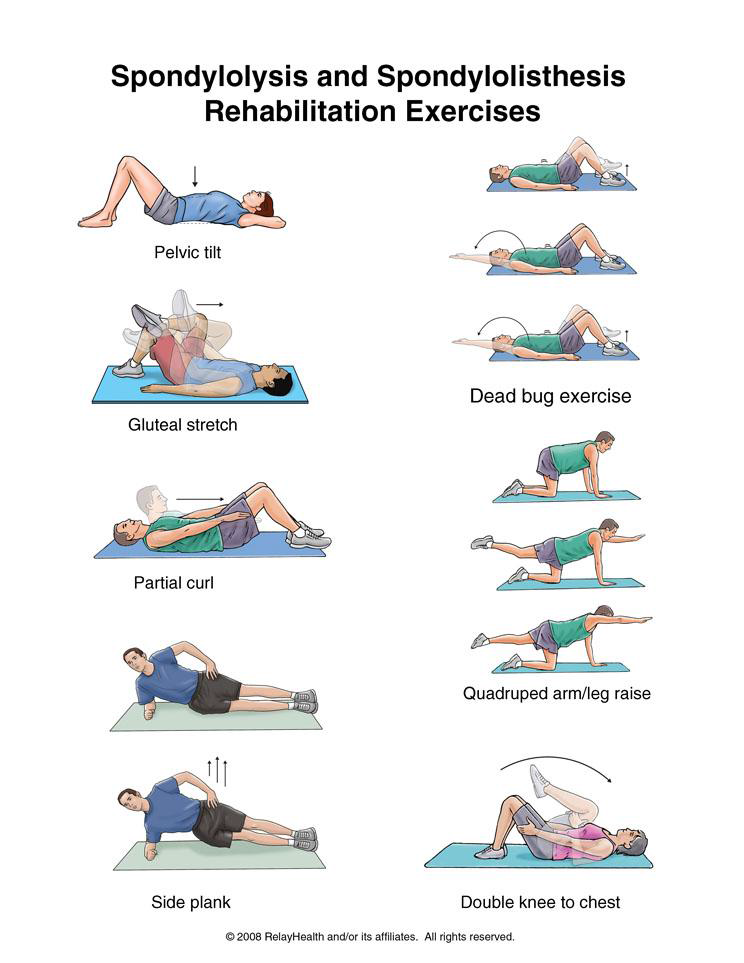
It is important to have strong abdominal muscles when the structures of your spine are weakened. These exercises help build strong stomach muscles.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
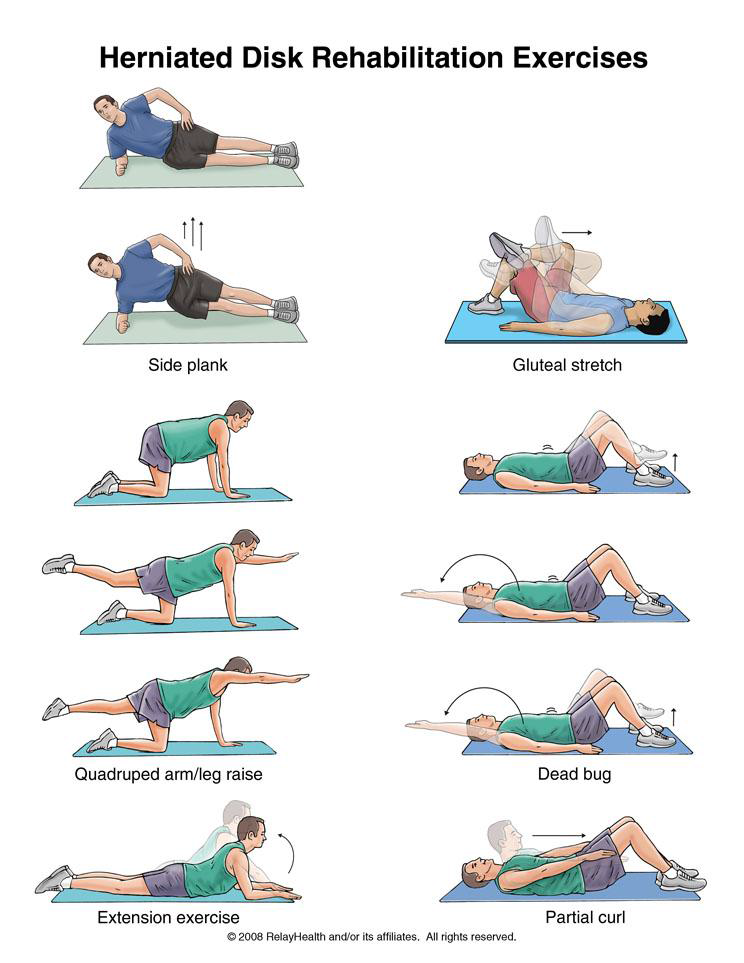
After lying on your stomach for 5 minutes, prop yourself up on your elbows for another 5 minutes. Lie flat again for 1 minute, then press down on your hands and extend your elbows while keeping your hips flat on the floor. Hold for 1 second and lower yourself to the floor. Repeat 10 times. Do 4 sets. Rest for 2 minutes between sets. You should have no pain in your legs when you do this, but it is normal to feel pain in your lower back. Do this several times a day.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
After lying on your stomach for 5 minutes, prop yourself up on your elbows for another 5 minutes. Lie flat again for 1 minute, then press down on your hands and extend your elbows while keeping your hips flat on the floor. Hold for 1 second and lower yourself to the floor. Repeat 10 times. Do 4 sets. Rest for 2 minutes between sets. You should have no pain in your legs when you do this, but it is normal to feel pain in your lower back. Do this several times a day.
Do the following, partial curl exercise only when you no longer have pain in your buttocks or legs.
If you have a herniated disk, you should limit driving and other sitting activities to no more than 30 minutes at a time. Walking is also good exercise for you.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
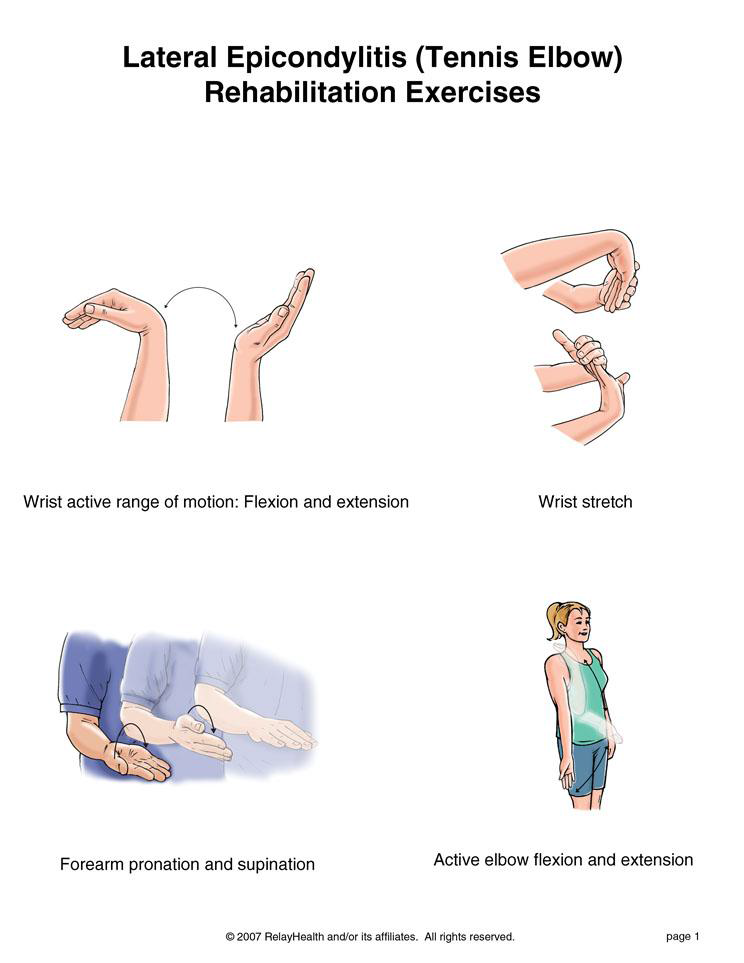
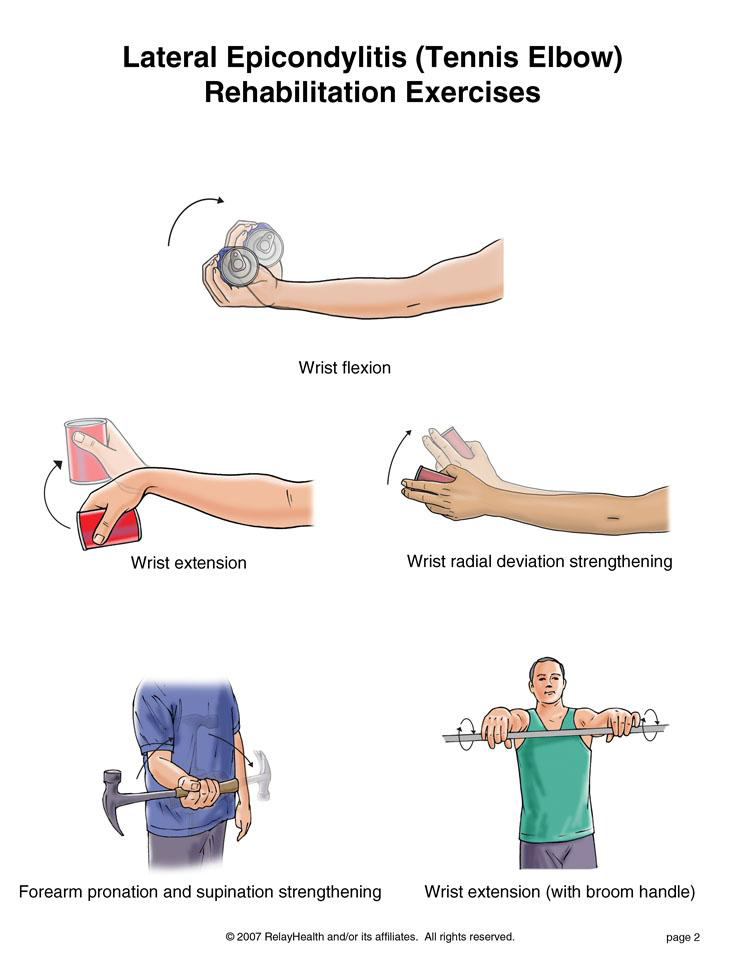
The first 5 exercises are stretching exercises. You may do these when the sharp wrist pain goes away. The last 3 exercises are strengthening exercises. You may do these exercises when stretching is nearly painless.
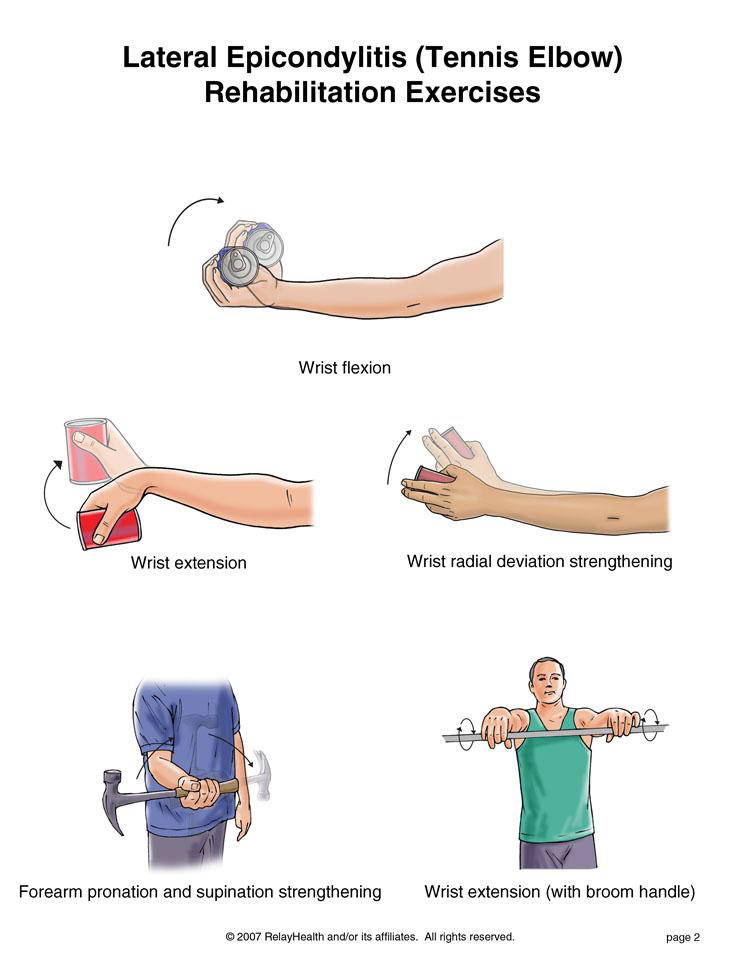
When this exercise becomes pain free, do it with some weight in your hand such as a soup can or hammer handle.
starting position. Do 3 sets of 10. Gradually increase the weight of the object you are holding.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
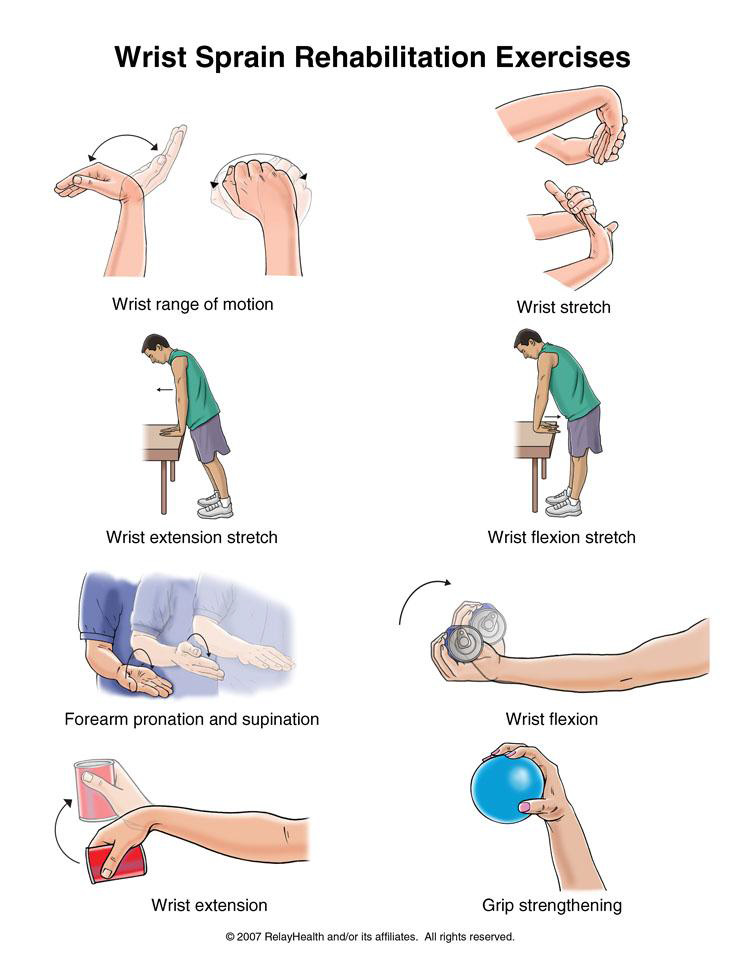
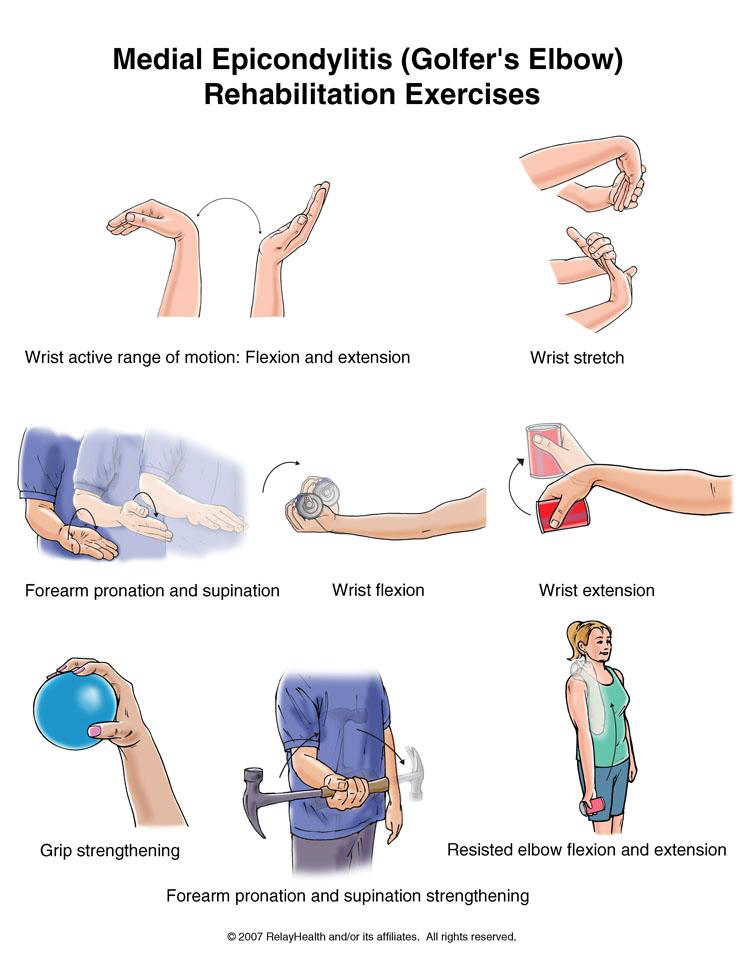
You may do the stretching exercises when the sharp wrist pain goes away. You may do the strengthening exercises when stretching is nearly painless.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
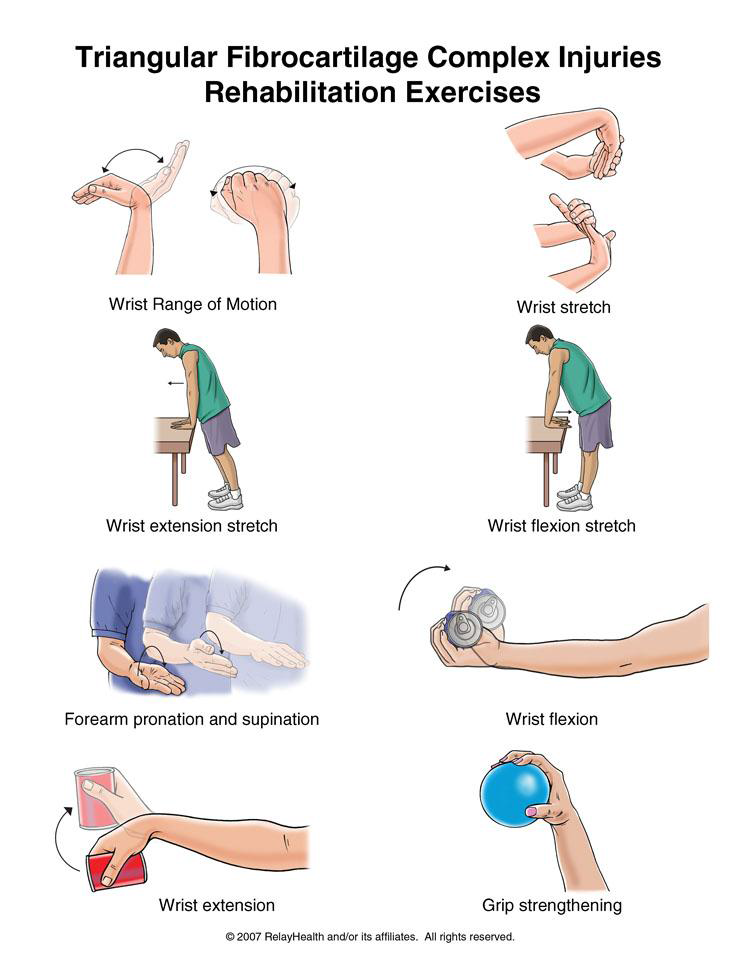
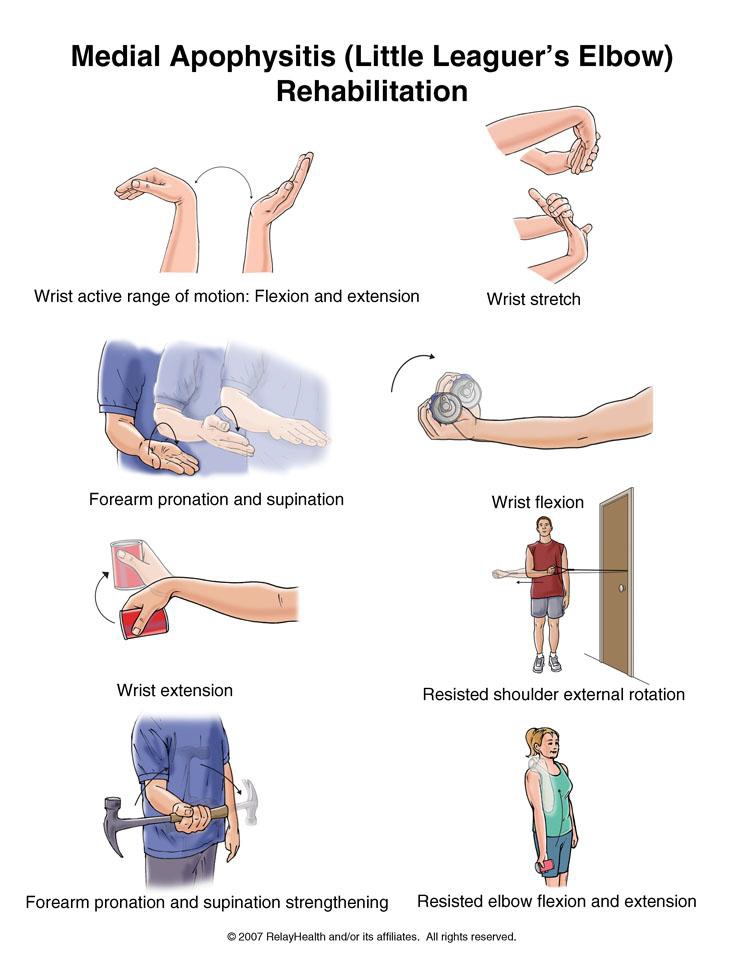
You may do all of these exercises when the initial pain is gone.
Written by Scott Coleman, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
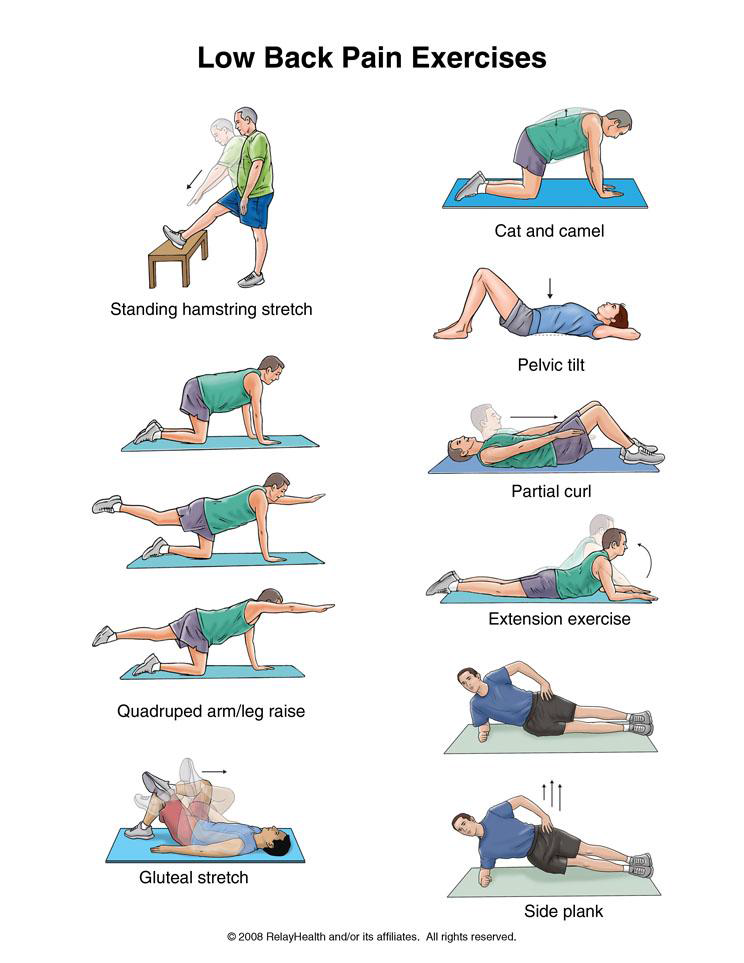
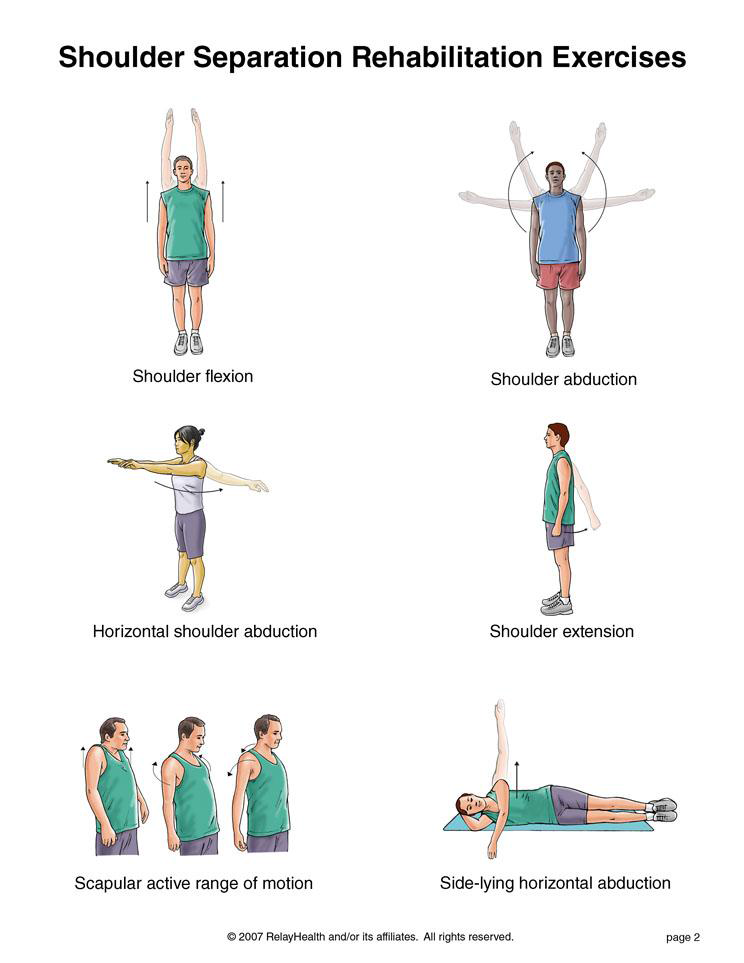
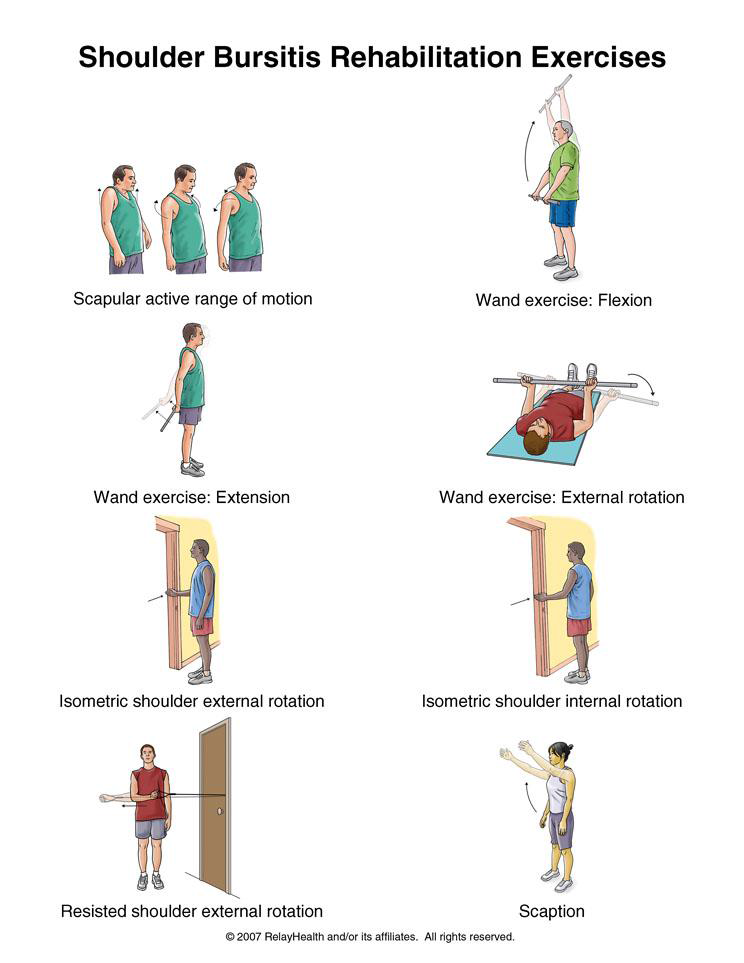
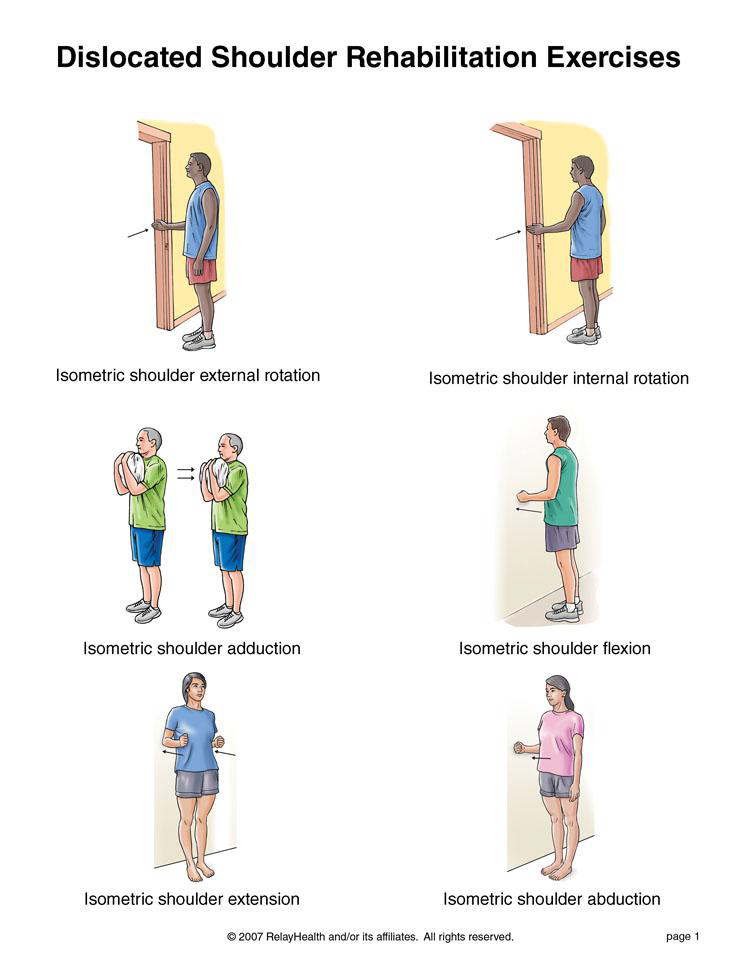
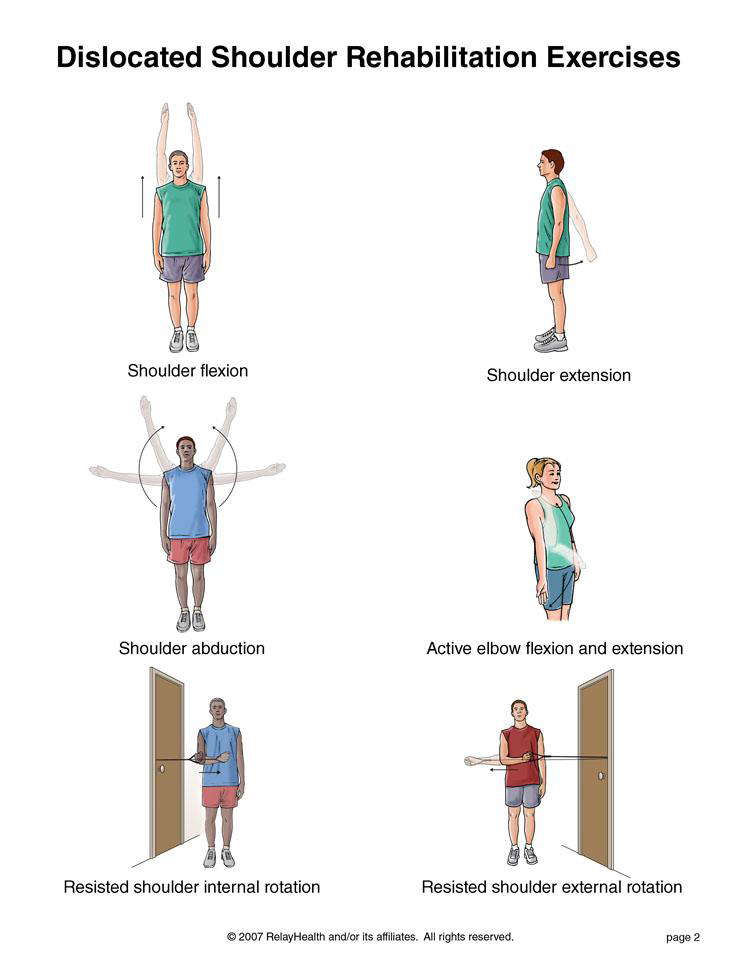
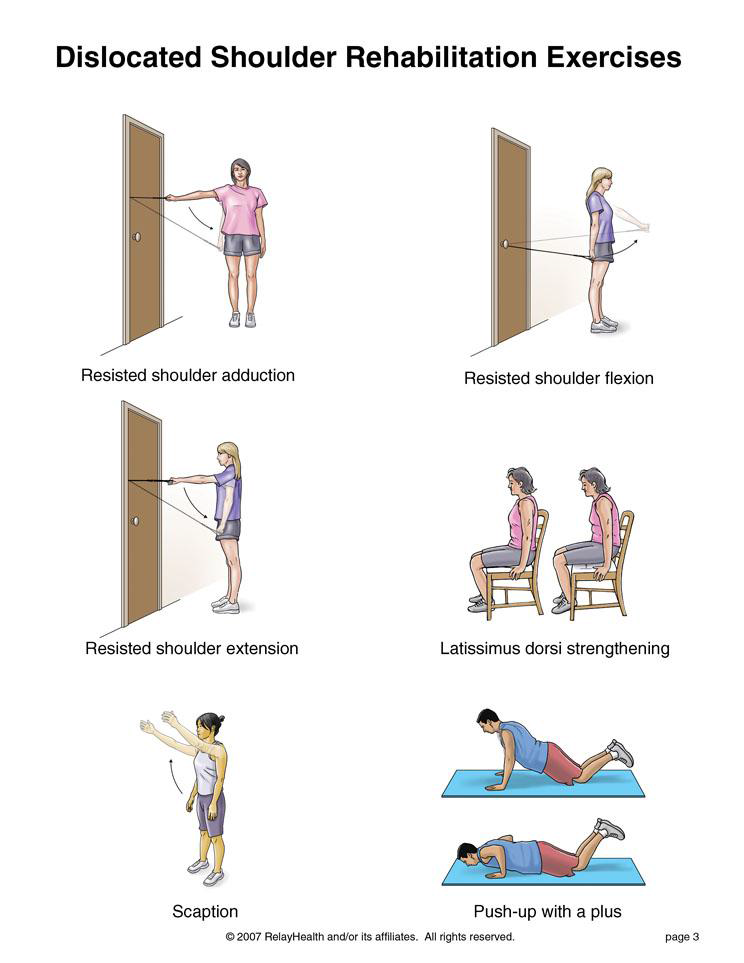
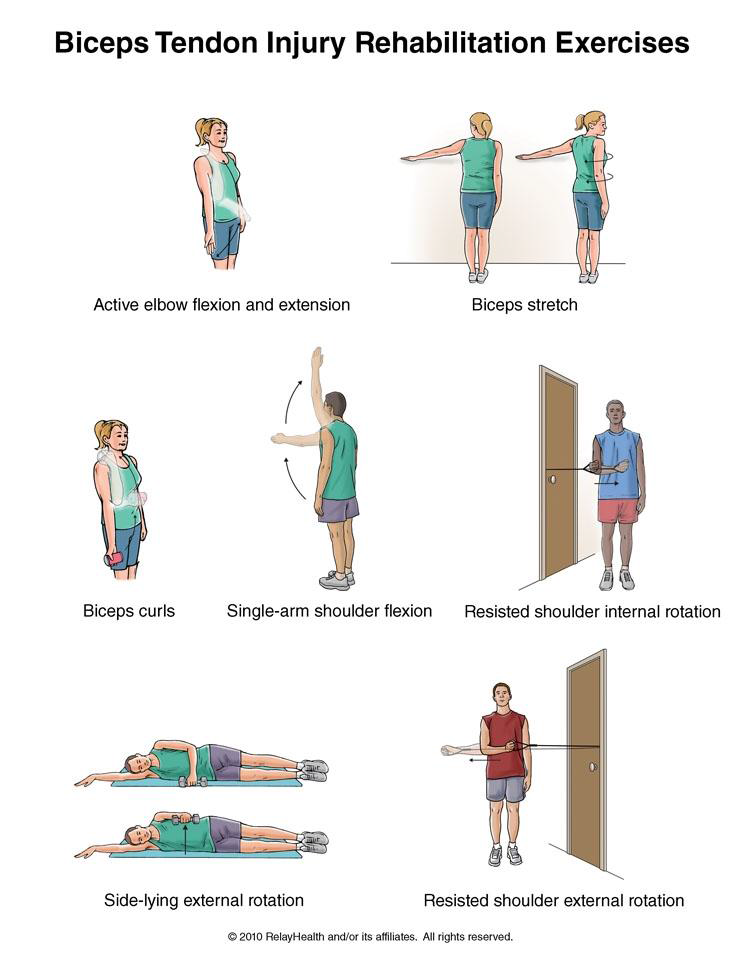
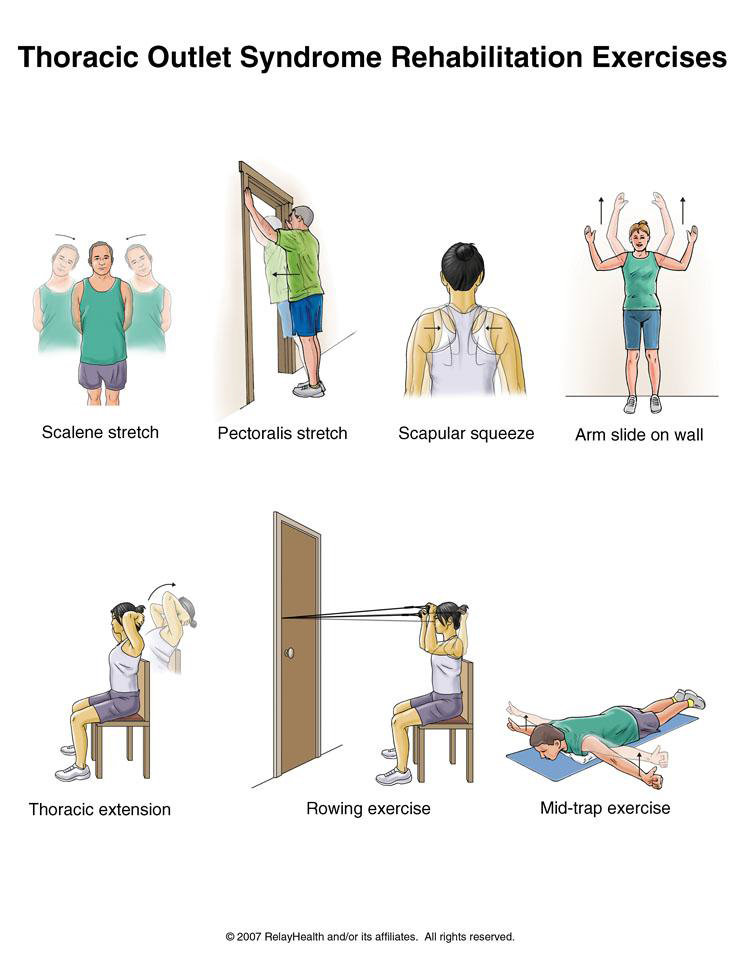
You may do the stretching exercises right away. You may do the strengthening exercises when stretching is nearly painless.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
You may do the stretching exercises right away. You may do the strengthening exercises when stretching is nearly painless.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
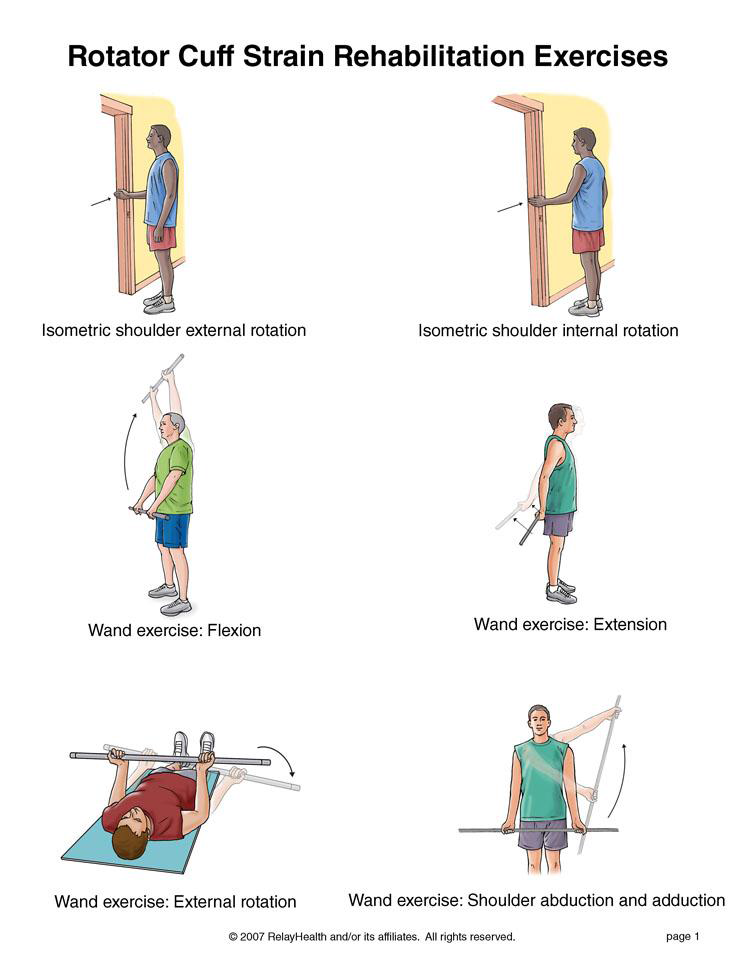
You may do the stretching exercises right away. You may do the strengthening exercises when stretching is nearly painless.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
You may do the stretching exercises right away. You may do the strengthening exercises when stretching is nearly painless.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
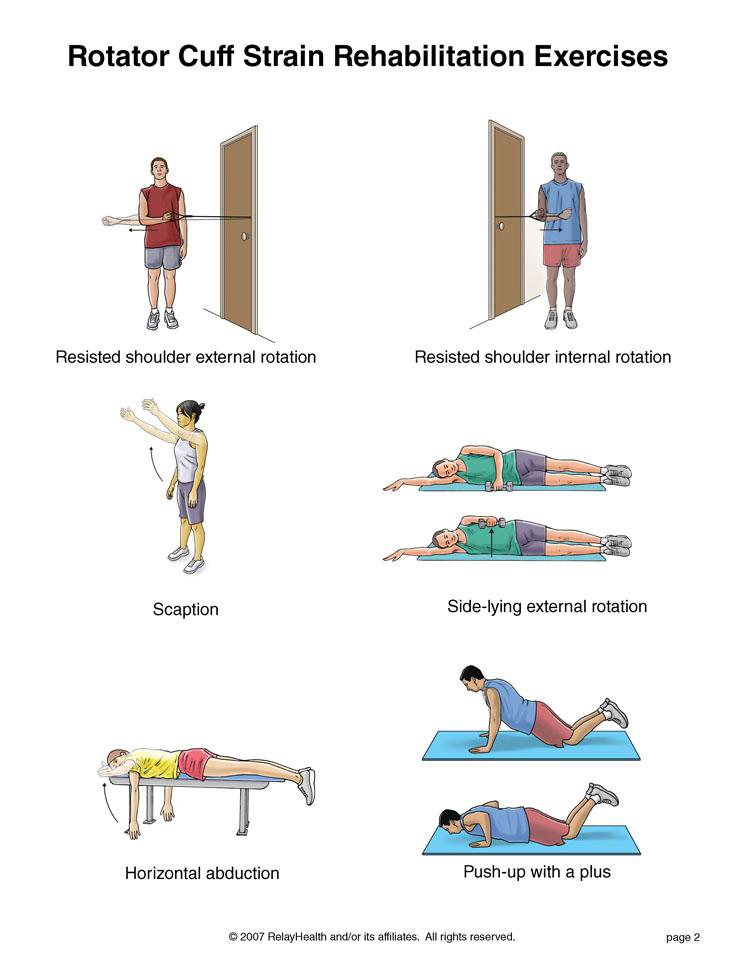
until the dumbbells touch. Lower slowly back to the starting position. Do 3 sets of 10. Gradually increase the amount of weight in your hands.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
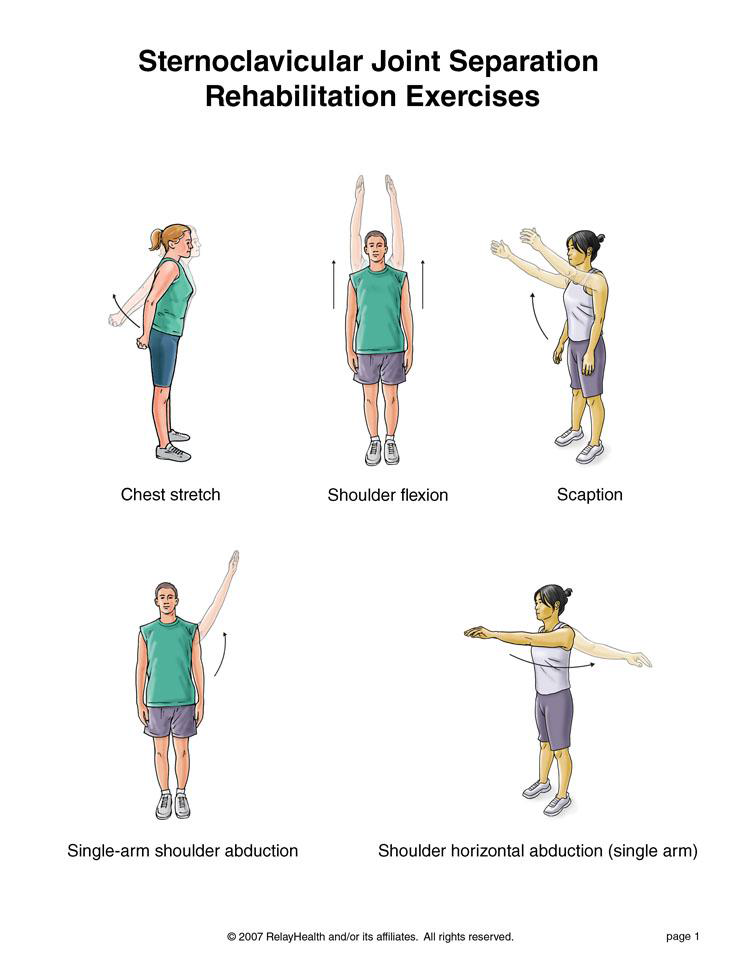
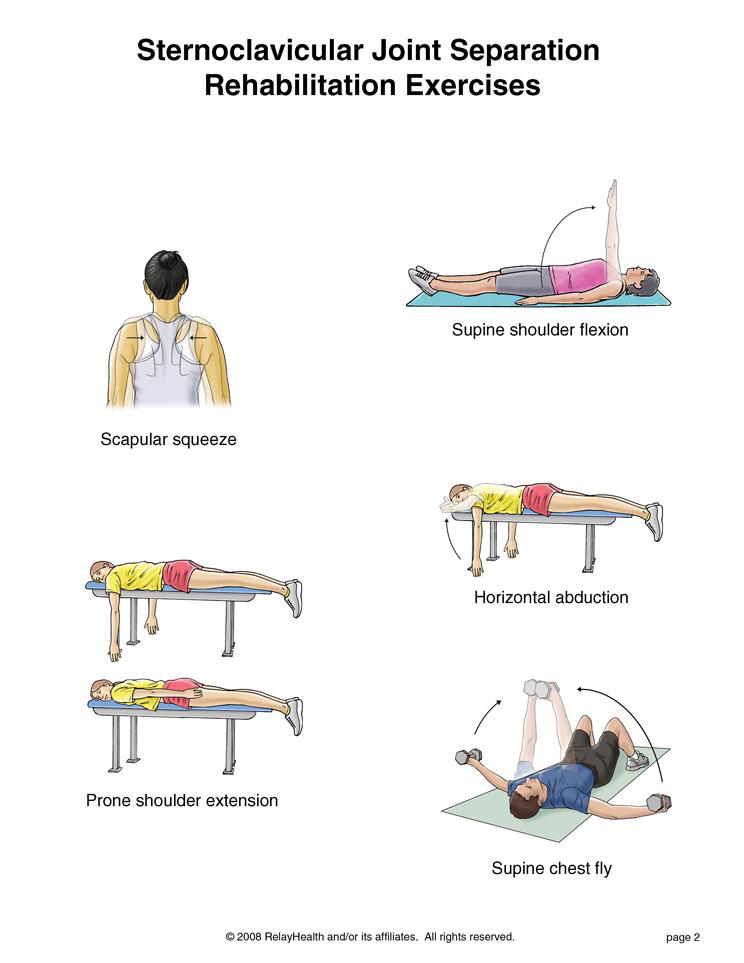
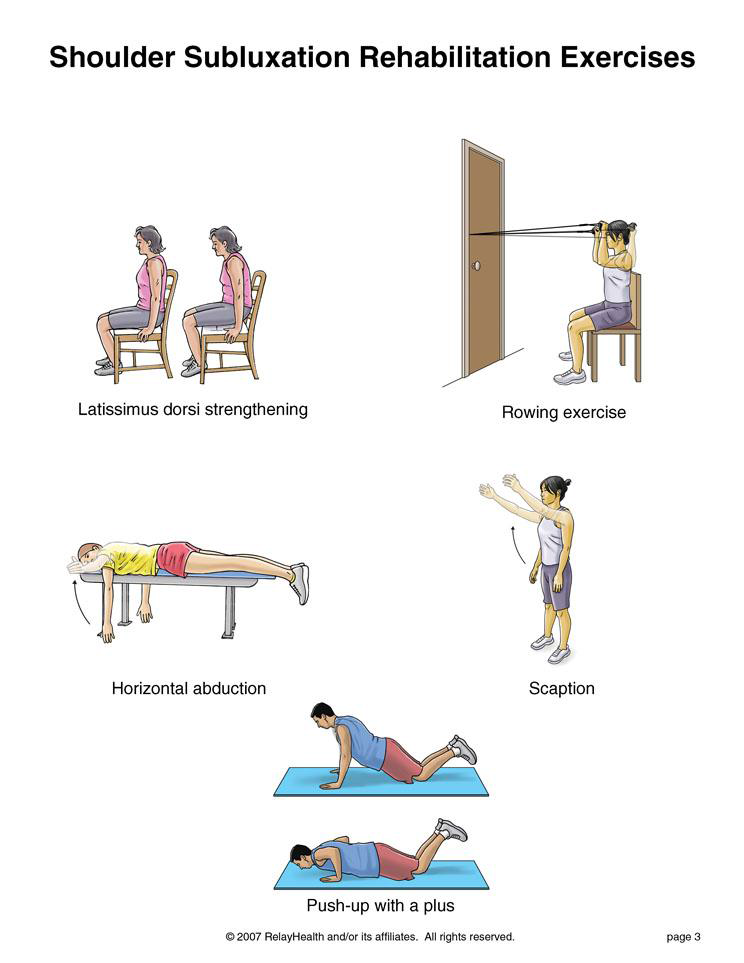
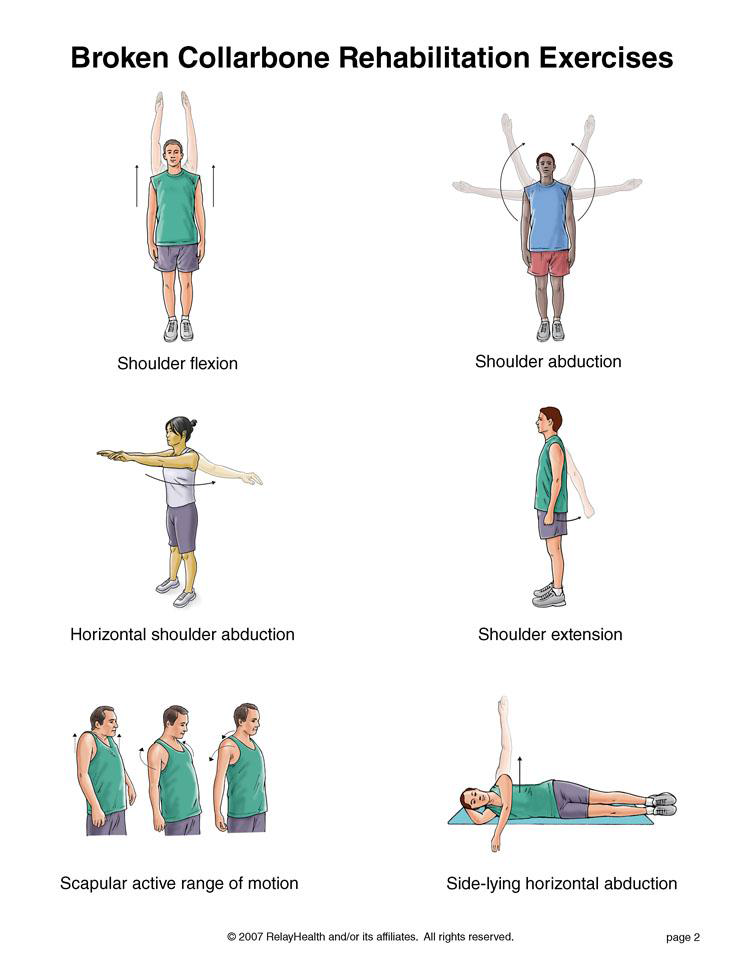
Do these exercises as soon as your healthcare provider says you can.
As these exercises become easier, add a weight to your hand to give you some resistance
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
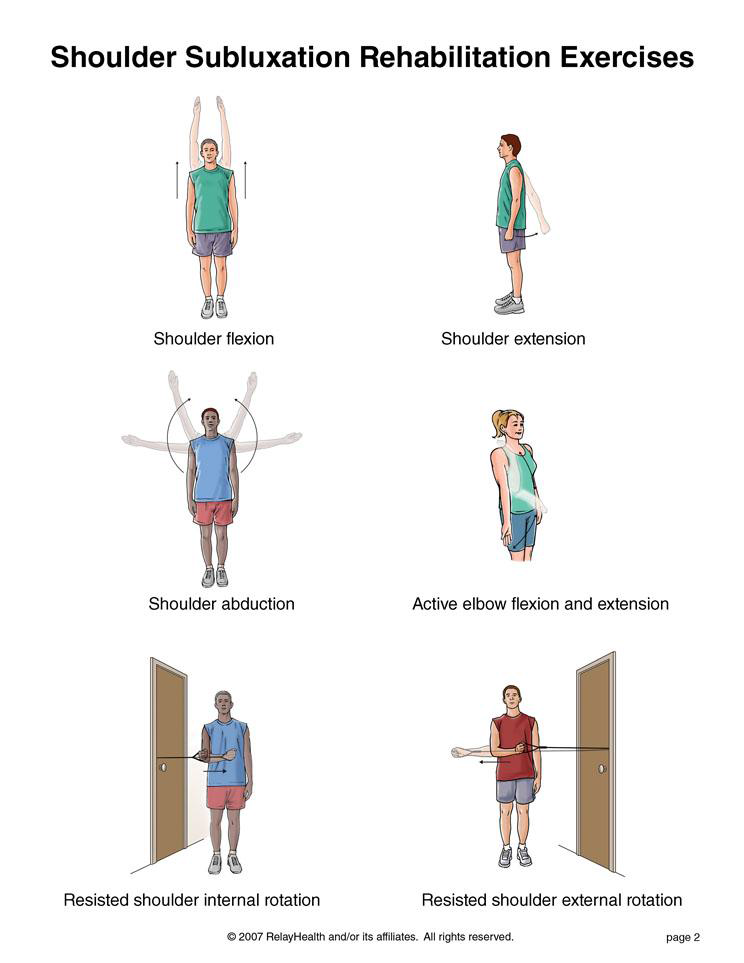
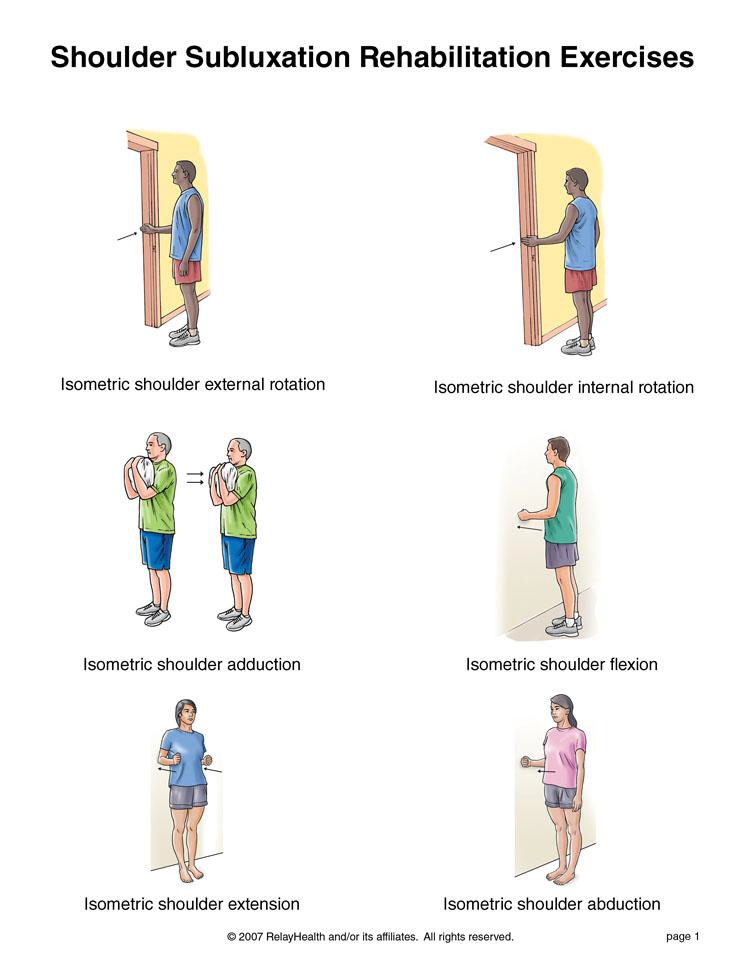
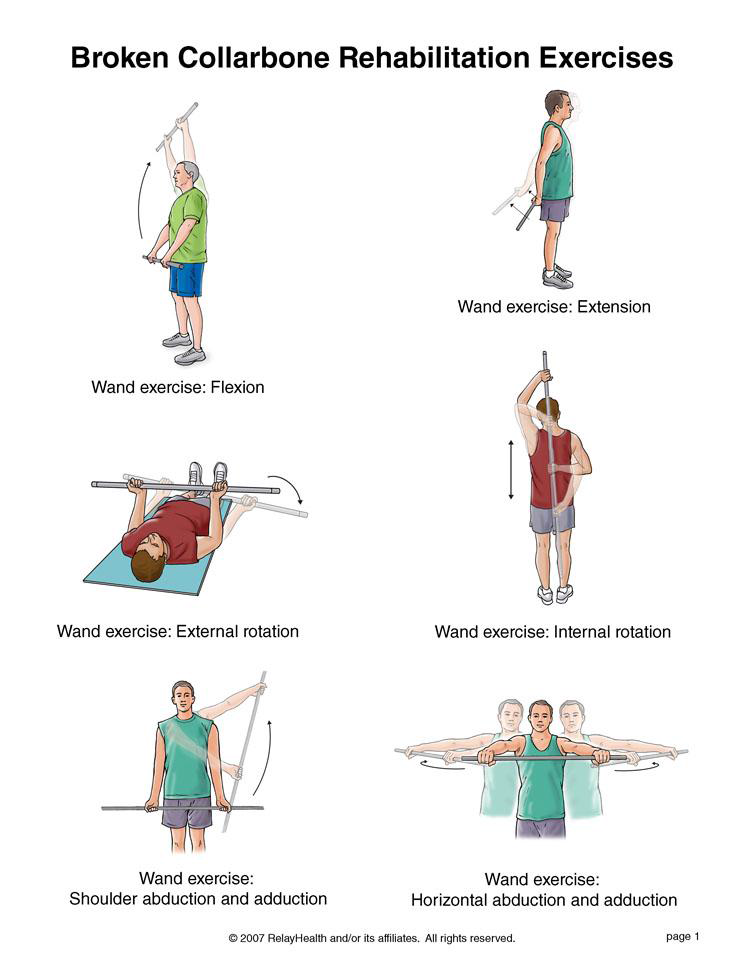
You may do these exercises when your pain has improved.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
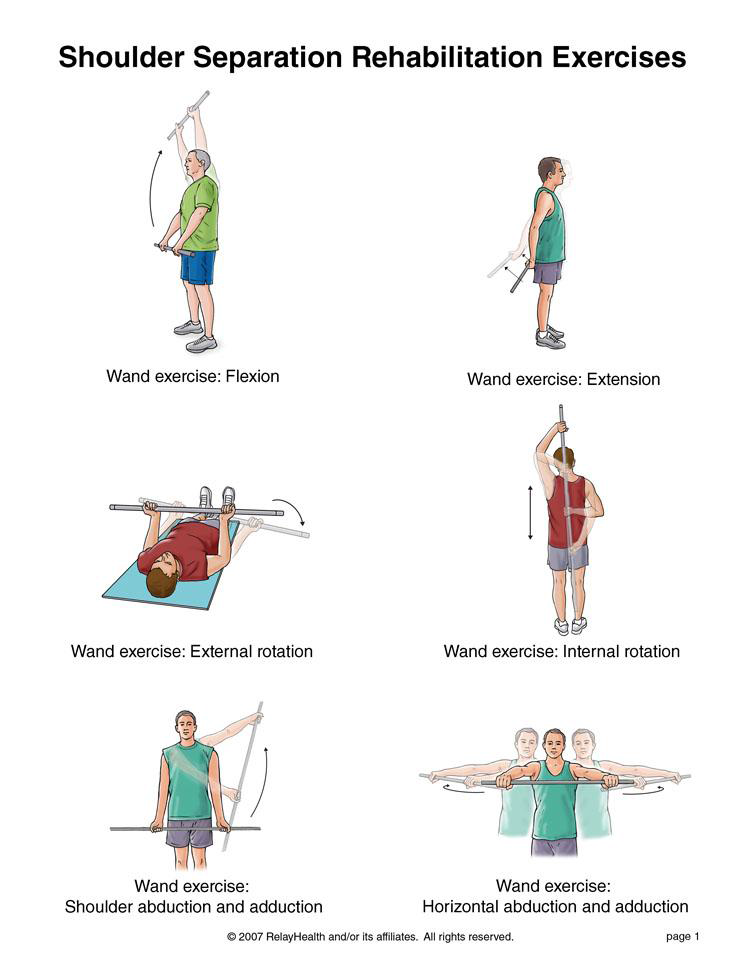
You may do all of these exercises right away.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
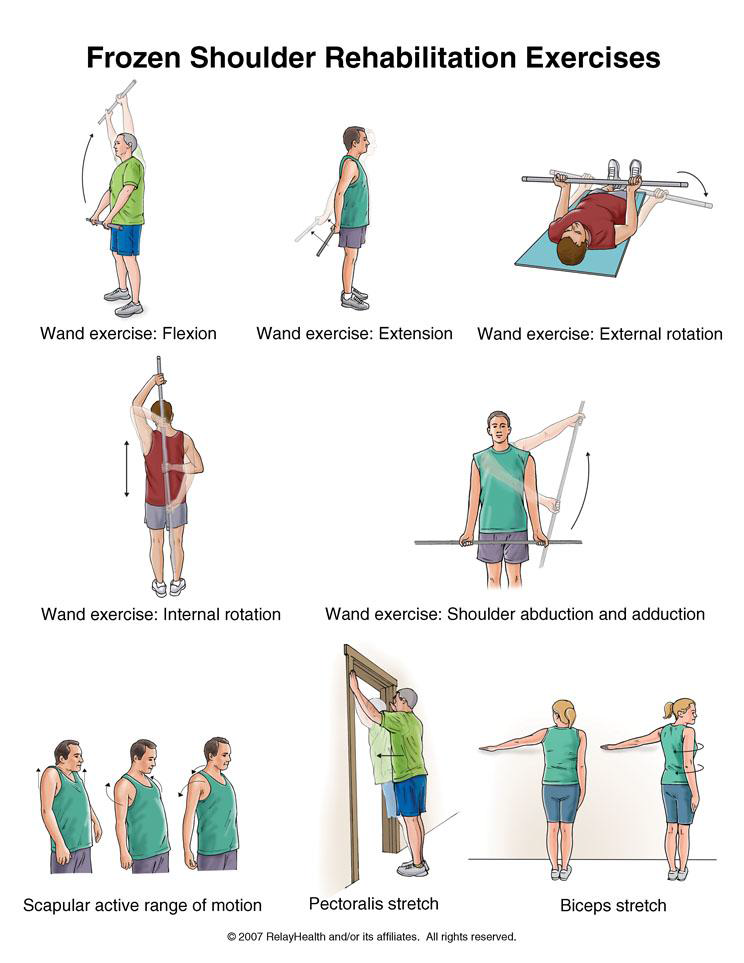
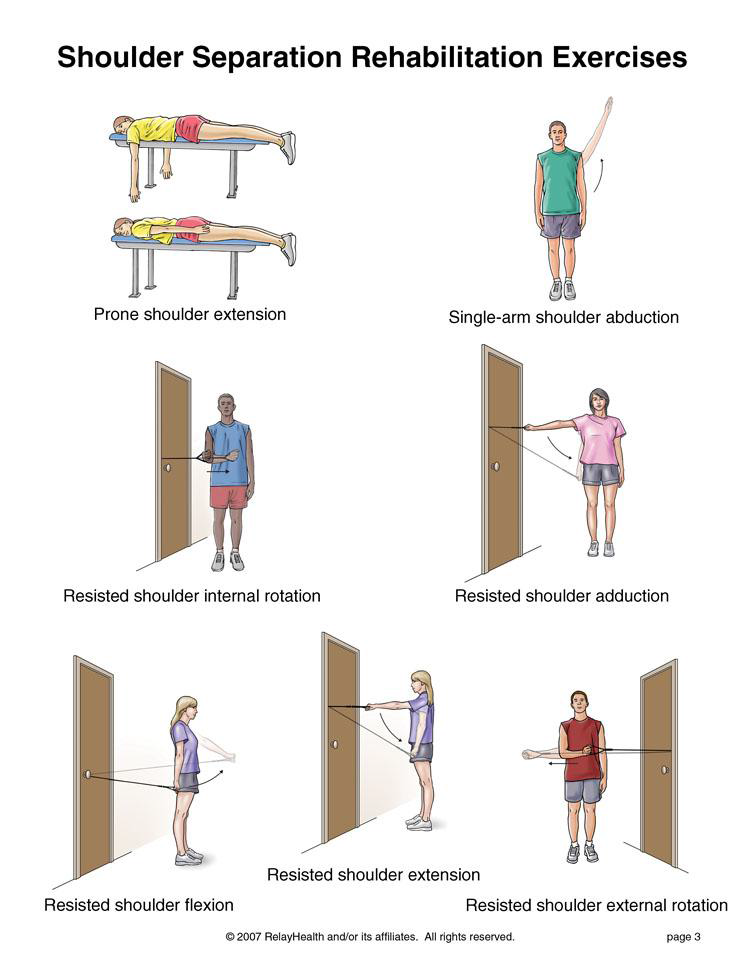
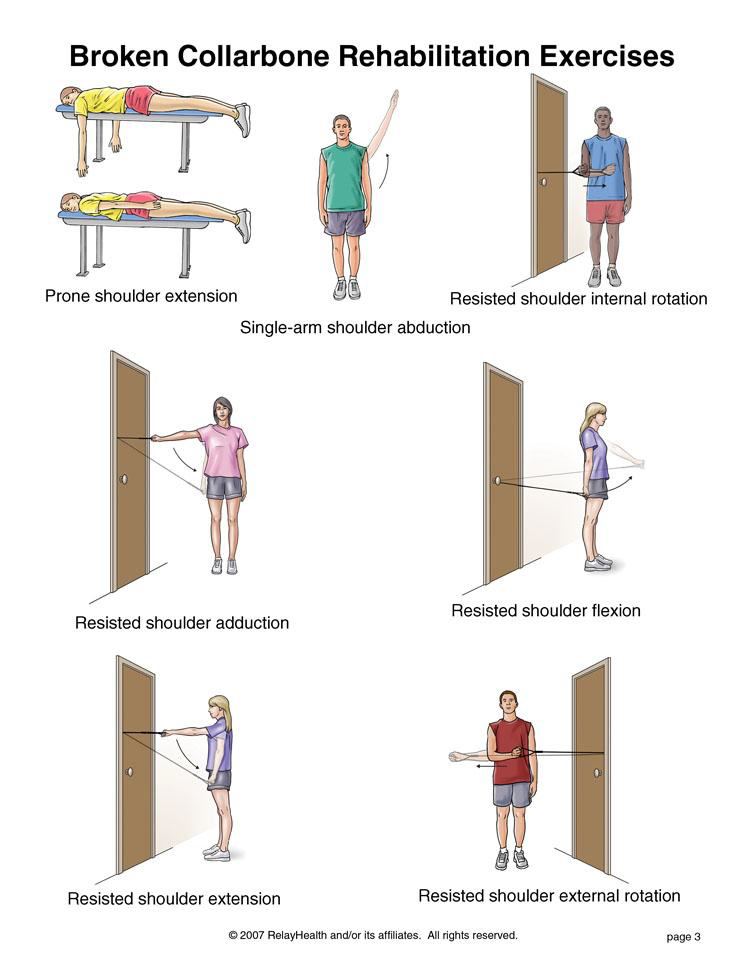
Do these exercises as soon as your healthcare provider says you can.
As these exercises become easier, add a weight to your hand to give you some resistance.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
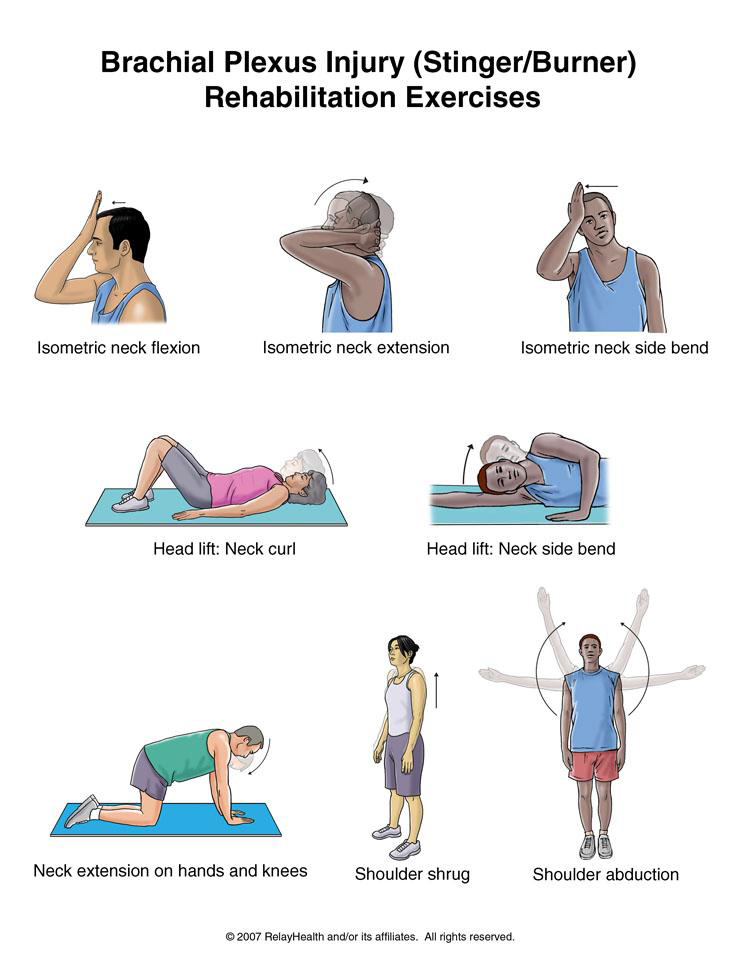
You can begin these exercises when moving your neck in all directions (up, down, right, left) does not cause numbness or tingling down your arm or into your hand. Do not do any exercises that make your neck pain worse.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
Written by Phyllis Clapis, PT, DHSc, OCS, and Pierre Rouzier, MD.
Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
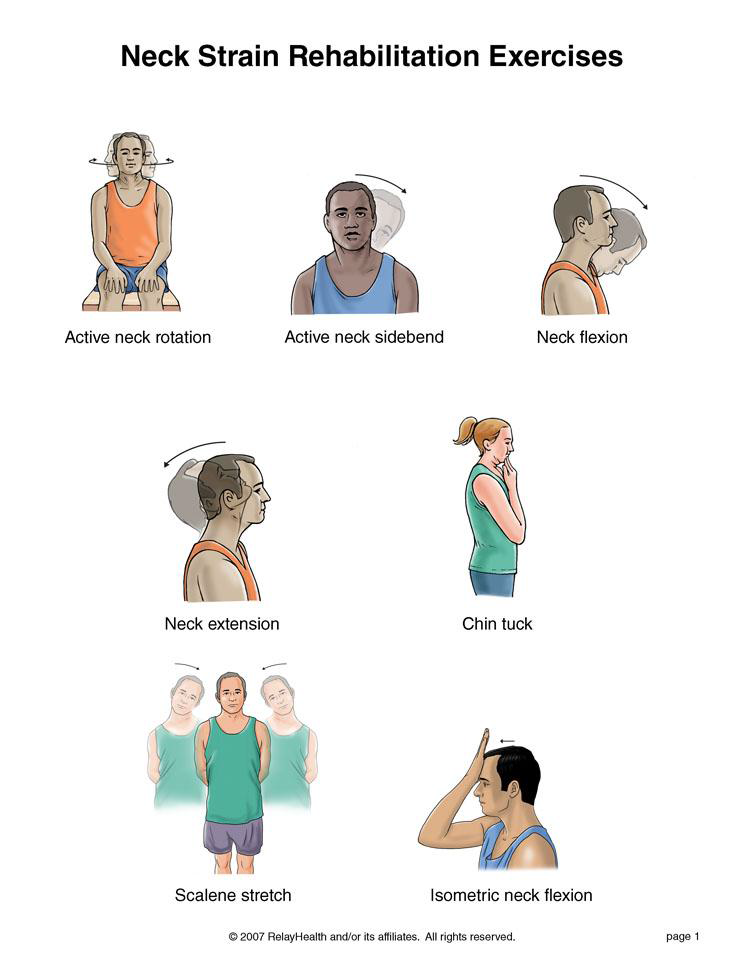
Do these exercises only if you do not have pain or numbness running down your arm or into your hand. The first 6 exercises are meant to help your neck remain flexible. Do not do any exercises that make your neck pain worse.
Written by Tammy White, MS, PT, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth. Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
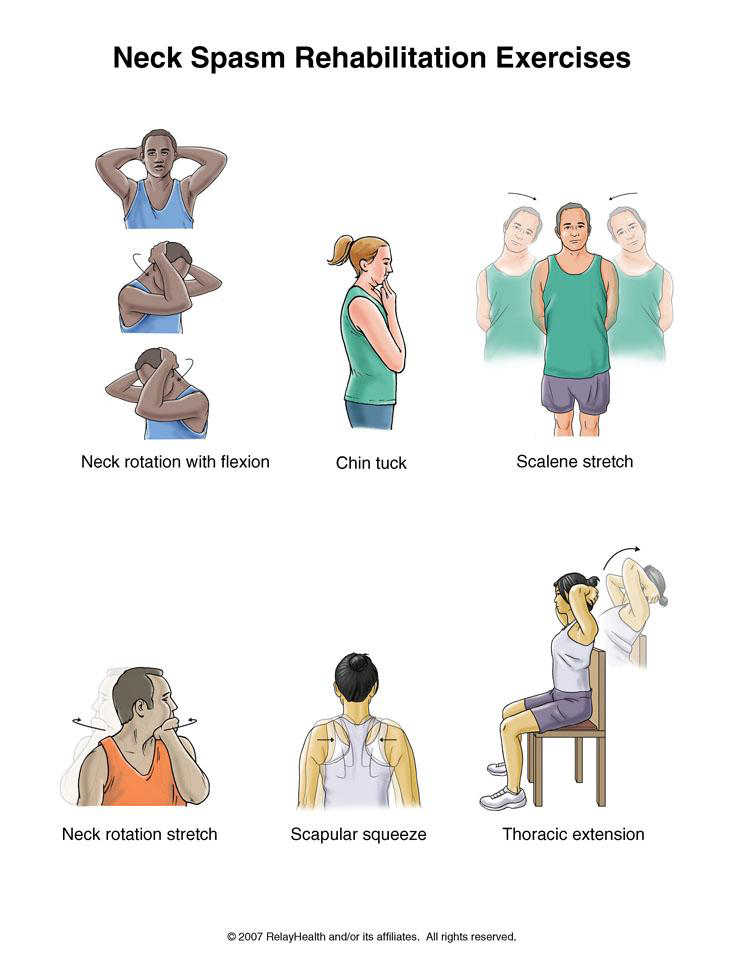
You may do all of these exercises right away but avoid any movements that increase your pain.
Right: Turn your head to the right and clasp your hands behind your head. Let the weight of your arms pull your chin to the right side of your chest. Relax. Hold for a count of 15. Do this 3 times.
Left: Turn your head to the left and clasp your hands behind your head. Let the weight of your arms pull your chin to the left side of your chest. Relax. Hold for a count of 15. Do this 3 times.
Right side: Rotate your neck by looking over your right shoulder. Lift your right hand and place your palm on the left side of your chin. Push your chin with your palm toward your right shoulder. Hold for a count of 10. Do this 3 times.
Left side: Rotate your neck by looking over your left shoulder. Lift your left hand and place your palm on the right side of your chin. Push your chin with your palm toward your left shoulder. Hold for a count of 10. Do this 3 times.
Written by Pierre Rouzier, MD, and Phyllis Clapis, PT, DHSc, OCS, for RelayHealth. Published by RelayHealth.
© 2009 RelayHealth and/or its affiliates. All Rights Reserved.
Wellness isn’t just a buzzword; it’s a holistic approach to health that encompasses physical, mental, and emotional well-being. While genetics play a role in determining our health outcomes, lifestyle factors such as diet, exercise, sleep, stress management, and social connections exert profound effects on our physiology. In this comprehensive guide, we’ll explore the intricate relationship between wellness practices and human physiology, shedding light on the underlying mechanisms through which lifestyle choices impact our bodies at the molecular, cellular, and systemic levels.
The food we eat serves as fuel for our bodies, providing the essential nutrients needed for energy production, cellular function, and tissue repair. A balanced diet rich in whole foods, fruits, vegetables, lean proteins, and healthy fats supports optimal physiological functioning while reducing the risk of chronic diseases such as obesity, diabetes, and cardiovascular disorders. Carbohydrates, proteins, and fats are macronutrients that undergo digestion and metabolism to generate ATP (adenosine triphosphate), the body’s primary energy currency. Macronutrient balance, along with micronutrient intake (vitamins, minerals, antioxidants), influences metabolic processes, hormone regulation, and immune function.
Regular exercise is not only essential for maintaining a healthy weight and cardiovascular health but also exerts profound effects on physiological systems throughout the body. Aerobic exercise, such as running, cycling, and swimming, improves cardiovascular fitness, enhances oxygen delivery to tissues, and stimulates the release of endorphins, neurotransmitters that promote mood elevation and stress reduction. Strength training exercises, meanwhile, increase muscle mass, bone density, and metabolic rate, contributing to overall strength, mobility, and metabolic health. Exercise-induced adaptations include improvements in insulin sensitivity, lipid profile, blood pressure, and inflammatory markers, reducing the risk of metabolic syndrome and chronic inflammation.
Quality sleep is essential for physical and mental well-being, serving as a time for rest, repair, and rejuvenation. During sleep, the body undergoes essential physiological processes, including tissue regeneration, hormone regulation, memory consolidation, and immune system modulation. Disruptions to the sleep-wake cycle, such as sleep deprivation or irregular sleep patterns, can impair cognitive function, mood stability, and metabolic health. Chronic sleep disturbances have been linked to an increased risk of obesity, insulin resistance, hypertension, and mood disorders.
Chronic stress triggers a cascade of physiological responses, including the release of stress hormones such as cortisol and adrenaline, activation of the sympathetic nervous system (fight-or-flight response), and suppression of the parasympathetic nervous system (rest-and-digest response). Prolonged stress exposure can dysregulate hormone levels, suppress immune function, and contribute to systemic inflammation, increasing the risk of stress-related disorders such as anxiety, depression, insomnia, and gastrointestinal problems. Mind-body practices such as meditation, deep breathing, yoga, and progressive muscle relaxation promote relaxation, activate the parasympathetic nervous system, and mitigate the detrimental effects of chronic stress on physiology.
Human beings are social creatures wired for connection, and interpersonal relationships play a crucial role in shaping our physiological responses to stress, adversity, and life events. Strong social support networks have been associated with better mental health, immune function, and longevity, while social isolation and loneliness are risk factors for poor health outcomes and mortality. Positive social interactions release feel-good neurotransmitters such as oxytocin and dopamine, which promote bonding, trust, and emotional resilience. Cultivating meaningful relationships, engaging in social activities, and seeking support from friends, family, and community networks are essential for nurturing emotional well-being and maintaining physiological equilibrium.
The practice of wellness encompasses a range of lifestyle choices and behaviors that profoundly influence human physiology at multiple levels. From nutrition and exercise to sleep, stress management, and social connections, each aspect of wellness plays a unique role in promoting optimal health and vitality. By adopting healthy habits and prioritizing self-care, individuals can harness the power of lifestyle medicine to optimize physiological function, prevent chronic disease, and enhance overall quality of life. Remember, wellness is not a destination but a journey, and each positive choice brings us closer to achieving our full potential for health and well-being.
Suffering an injury can be a challenging and often disheartening experience, impacting not only physical health but also emotional well-being and overall quality of life. Whether it’s a sprained ankle, a torn ligament, or a post-surgery rehabilitation, the journey to recovery can feel daunting. However, with the guidance and expertise of physical therapists, individuals can navigate this journey with confidence and resilience. In this comprehensive guide, we’ll explore the critical role of physical therapy in the rehabilitation process, from reducing pain and restoring mobility to enhancing strength and preventing future injuries.
Physical therapy is a branch of rehabilitative health focused on restoring movement and function following injury, illness, or surgery. Physical therapists are highly trained healthcare professionals who assess, diagnose, and treat musculoskeletal and movement disorders using evidence-based techniques and interventions.
Pain Management: Physical therapists employ various modalities such as manual therapy, therapeutic exercises, electrical stimulation, and ultrasound to alleviate pain and discomfort associated with injury or surgery.
Restoring Mobility and Function: Through targeted exercises, stretches, and manual techniques, physical therapists work to improve joint range of motion, flexibility, and functional abilities, enabling individuals to perform activities of daily living with greater ease and confidence.
Strengthening and Conditioning: Physical therapy programs often include strength training exercises to rebuild weakened muscles, improve muscle balance, and enhance overall physical fitness, reducing the risk of reinjury.
Improving Balance and Coordination: Balance and coordination are essential for safe movement and injury prevention. Physical therapists incorporate balance exercises, proprioceptive training, and coordination drills to enhance motor control and reduce the risk of falls.
Education and Empowerment: Physical therapists educate patients about their condition, treatment options, and injury prevention strategies, empowering them to take an active role in their recovery and long-term health.
The Role of Physical Therapy After Injury
After sustaining an injury, whether acute or chronic, seeking prompt physical therapy intervention is crucial for optimal recovery and long-term outcomes. Here’s how physical therapy can benefit individuals at different stages of the rehabilitation process:
During the acute phase of injury, immediate goals focus on reducing pain, swelling, and inflammation while protecting the injured area from further damage. Physical therapists may employ modalities such as ice, compression, and elevation (R.I.C.E), along with gentle range-of-motion exercises to maintain joint mobility and prevent stiffness.
As the acute symptoms subside, physical therapy interventions become more focused on restoring function and mobility. Physical therapists develop personalized treatment plans tailored to the individual’s specific needs, incorporating a combination of manual therapy techniques, therapeutic exercises, and functional activities to promote healing and rehabilitation.
In the later stages of rehabilitation, the emphasis shifts towards rebuilding strength, improving flexibility, and enhancing overall physical performance. Physical therapists prescribe progressive exercise programs designed to address muscle imbalances, restore functional movement patterns, and optimize biomechanics, facilitating a safe return to pre-injury activities and sports.
Even after completing formal physical therapy, maintaining an active lifestyle and adhering to a personalized home exercise program are essential for preventing re-injury and promoting long-term musculoskeletal health. Physical therapists provide education on proper body mechanics, ergonomics, and injury prevention strategies to empower individuals to stay healthy and active.
Physical therapy plays a vital role in the rehabilitation journey following injury, providing individuals with the support, guidance, and expertise needed to recover safely and effectively. By addressing pain, restoring mobility, enhancing strength, and promoting overall wellness, physical therapists empower individuals to overcome adversity, reclaim their independence, and live life to the fullest. Remember, the road to recovery may be challenging, but with perseverance, determination, and the right team by your side, healing and renewal are possible.
Chukwuemeka Nnabuife MD, DO CAQ
In a world where fad diets and quick fixes dominate headlines, achieving sustainable weight loss can feel like an elusive goal. However, by understanding the science behind weight loss and adopting evidence-based strategies, you can embark on a journey towards a healthier lifestyle that lasts a lifetime. In this comprehensive guide, we’ll delve into the intricacies of weight loss, exploring the physiological factors at play, debunking common myths, and providing actionable tips to help you achieve your goals.
At its core, weight loss is a simple equation: calories consumed versus calories expended. To lose weight, you need to create a calorie deficit, which means consuming fewer calories than your body uses for energy. However, the human body is a complex system influenced by various factors, including metabolism, hormones, genetics, and behavior.
Metabolism, often misunderstood, refers to the process by which your body converts food and drink into energy. Basal metabolic rate (BMR) accounts for the majority of calories burned at rest, while physical activity and the thermic effect of food also contribute to energy expenditure.
Hormones play a crucial role in regulating appetite, metabolism, and fat storage. Hormones like insulin, leptin, ghrelin, and cortisol influence hunger, satiety, and fat metabolism, making hormonal balance essential for weight management.
Genetics can predispose individuals to certain body types and metabolic rates, but they do not dictate destiny. While genetics may influence weight loss outcomes to some extent, lifestyle factors like diet and exercise play a more significant role in determining success.
Before diving into effective weight loss strategies, it’s essential to dispel common myths that often derail progress:
Myth 1: Crash diets lead to sustainable weight loss. Reality: Crash diets may result in rapid initial weight loss, but they are unsustainable and often lead to rebound weight gain.
Myth 2: Carbohydrates are the enemy. Reality: Carbohydrates are a vital source of energy and essential for overall health. The key is to choose complex carbohydrates like whole grains, fruits, and vegetables while moderating intake of refined sugars and processed foods.
Myth 3: You have to exercise excessively to lose weight. Reality: While exercise is beneficial for weight loss and overall health, it’s not necessary to spend hours at the gym every day. Consistent, moderate exercise combined with dietary changes yields the best results.
Now that we’ve laid the foundation, let’s explore science-backed strategies for achieving sustainable weight loss.
Set Realistic Goals: Instead of fixating on a specific number on the scale, focus on adopting healthier habits that promote long-term success. Set realistic, achievable goals based on behavior changes rather than strict weight targets.
Prioritize Nutrition: Opt for a balanced diet rich in whole foods, including lean proteins, fruits, vegetables, whole grains, and healthy fats. Practice portion control, mindful eating, and moderation rather than restrictive dieting.
Monitor Caloric Intake: Keep track of your food intake using a food diary or mobile app to gain insight into your eating habits and calorie consumption. Aim for a moderate calorie deficit of 500 to 750 calories per day to promote steady weight loss.
Stay Hydrated: Drink plenty of water throughout the day to stay hydrated and support metabolism. Sometimes thirst can be mistaken for hunger, leading to unnecessary calorie consumption.
Incorporate Physical Activity: Find enjoyable forms of exercise that suit your lifestyle and preferences, whether it’s walking, cycling, swimming, or dancing. Aim for at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity per week, along with muscle-strengthening exercises on two or more days.
Get Adequate Sleep: Prioritize quality sleep, aiming for 7-9 hours per night. Lack of sleep can disrupt hormone levels, increase appetite, and hinder weight loss efforts.
Manage Stress: Practice stress-reducing techniques such as mindfulness, meditation, deep breathing, or yoga to minimize emotional eating and cortisol levels, which can promote abdominal fat storage.
Seek Support: Surround yourself with a supportive network of friends, family, or professionals who can offer encouragement, accountability, and guidance on your weight loss journey.
In conclusion, achieving sustainable weight loss requires a holistic approach that addresses diet, exercise, mindset, and lifestyle factors. By understanding the science behind weight loss, dispelling common myths, and implementing evidence-based strategies, you can embark on a journey towards improved health, vitality, and well-being. Remember, small, consistent changes over time can lead to significant and lasting results.
– By Dr. Nnabuife
45 min 190 US dollars
Experience relief from migraine pain and discomfort with our specialized Migraine Cocktail infusion. Carefully crafted to address the unique needs of migraine sufferers, this blend combines fluid, electrolytes, and essential B vitamins to replenish hydration levels and restore balance to your body.
Our Migraine Cocktail also includes a targeted migraine pain reliever to alleviate the intensity of headaches and provide immediate tension relief. Additionally, for those experiencing nausea alongside their migraines, we offer the option of including an anti-nausea medication to help ease gastrointestinal symptoms.
Designed to offer rapid relief and comfort during a migraine attack, our infusion provides comprehensive support to help you manage and overcome the challenges associated with migraines. Say goodbye to debilitating headaches and reclaim control over your well-being with our Migraine Cocktail infusion.
45 min 250 US dollars
Indulge in the ultimate personalized wellness experience with our Custom Cocktail service. Tailored to meet your unique needs and preferences, our exclusive drip offers a bespoke blend of vitamins, minerals, antioxidants, and symptom relievers, meticulously curated by our team of licensed medical practitioners.
Whether you’re seeking to boost your immune system, enhance energy levels, or alleviate specific symptoms, our Custom Cocktail service is designed to cater to your individual requirements. During a consultation with our experienced medical professionals, you’ll have the opportunity to discuss your wellness goals and concerns, allowing us to create a customized formula that addresses your specific needs.
With the flexibility to choose up to two add-ons, you can further tailor your infusion to suit your preferences and optimize your wellness journey. Experience the luxury of personalized care and embark on a path to enhanced vitality and well-being with our Custom Cocktail service. Your journey to optimal health starts here!
Arthritis refers to a group of inflammatory joint disorders characterized by pain, swelling, stiffness, and decreased range of motion. There are many types of arthritis, but the two most common forms are osteoarthritis (OA) and rheumatoid arthritis (RA).
Call the office or book an appointment online today.
Osteoarthritis (OA):
Rheumatoid Arthritis (RA):
Medications:
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen can help reduce pain and inflammation.
Disease-modifying antirheumatic drugs (DMARDs) are often prescribed for RA to suppress the immune system and slow disease progression.
Corticosteroids may be used to provide short-term relief of severe arthritis symptoms.
Analgesics such as acetaminophen can help alleviate pain but do not reduce inflammation.
Lifestyle Modifications:
Regular exercise, including low-impact activities like swimming or cycling, can help improve joint function and mobility.
Maintaining a healthy weight can reduce stress on weight-bearing joints and slow the progression of OA.
Physical therapy can provide exercises to strengthen muscles around the affected joints and improve flexibility.
Assistive devices such as braces, splints, or orthotic shoe inserts can help support the joints and alleviate pain.
Joint Protection:
Avoiding activities that exacerbate joint pain or cause further damage, such as high-impact sports or repetitive movements.
Using ergonomic tools and techniques to reduce joint stress during daily tasks.
Surgery:
Joint replacement surgery may be considered for severe OA or RA that does not respond to other treatments, particularly in the hips or knees.
Other surgical options include arthroscopy, synovectomy, or joint fusion to alleviate pain and improve joint function.
It’s important to work with a healthcare provider, such as a rheumatologist or orthopedic specialist, to develop a comprehensive treatment plan tailored to your specific type and severity of arthritis. Early intervention and appropriate management can help alleviate symptoms, preserve joint function, and improve quality of life for individuals with arthritis.
A concussion is a type of traumatic brain injury (TBI) caused by a sudden jolt, blow, or bump to the head or body that results in the brain’s rapid movement within the skull. This movement can cause stretching and damage to brain cells and disrupt normal brain function temporarily. Concussions are often referred to as mild TBIs because they are usually not life-threatening, but they can have serious short-term and long-term effects on cognitive, physical, and emotional health. Our sports medicine program includes specialized care for athletes who have sustained concussions or head injuries. Our sports medicine physicians are trained in concussion evaluation and management protocols, including sideline assessment, symptom monitoring, neurocognitive testing, and gradual return-to-play protocols. We prioritize the safety and well-being of athletes with concussions, providing comprehensive care to support their recovery and minimize the long-term effects of head injuries.
Call the office or book an appointment online today.
Symptoms of Concussion:
Headache or Pressure in the Head: The most common symptom of concussion is a headache, which may vary in intensity.
Dizziness or Balance Problems: Feeling dizzy, lightheaded, or unsteady on your feet is common after a concussion.
Nausea or Vomiting: Some individuals may experience nausea or vomiting after sustaining a concussion.
Confusion or Disorientation: Difficulty concentrating, feeling mentally foggy, or having trouble remembering events before or after the injury.
Sensitivity to Light or Noise: Increased sensitivity to light or noise, known as photophobia and phonophobia, respectively.
Visual Disturbances: Blurred or double vision, seeing stars, or difficulty focusing on objects.
Fatigue or Drowsiness: Feeling unusually tired, lethargic, or sleepy even after getting adequate rest.
Sleep Disturbances: Changes in sleep patterns, such as difficulty falling asleep, excessive sleepiness, or disrupted sleep.
Mood Changes: Irritability, mood swings, anxiety, depression, or emotional instability may occur following a concussion.
Memory Problems: Difficulty recalling recent events, difficulty concentrating, or feeling mentally sluggish.
It’s essential to seek medical attention if you or someone else experiences any of the following symptoms after a head injury:
Deteriorating mental status (confusion, agitation, difficulty waking up) Loss of consciousness: Although not all concussions involve loss of consciousness, if it does occur, especially for an extended period, it can indicate a more severe brain injury.
Worsening symptoms: If symptoms such as headache, dizziness, confusion, or nausea worsen over time rather than improving, it could suggest an evolving brain injury.
Seizures: Seizures following a head injury can be a sign of a more severe brain injury and require immediate medical attention.
Persistent vomiting: Vomiting that continues or worsens after the initial injury may indicate increased intracranial pressure and should be evaluated promptly.
Unequal pupil size: Also known as anisocoria, a significant difference in the size of the pupils can be a sign of serious brain injury or other neurological problems.
Severe or worsening headache: While headaches are common after a concussion if they are severe, persistent, or getting worse, it may indicate a more serious issue.
Weakness or numbness: Weakness or numbness, especially on one side of the body, can indicate damage to the brain or spinal cord and should be evaluated immediately.
Difficulty waking up: If someone has difficulty waking up or appears excessively drowsy after a head injury, it could indicate a more severe brain injury.
Confusion or agitation: Severe confusion, unusual behavior, or agitation following a head injury may be signs of a more severe brain injury.
Slurred speech: Difficulty speaking clearly, or slurred speech can be a sign of neurological impairment and should be evaluated promptly.
The primary treatment for concussion involves rest and avoiding activities that may exacerbate symptoms. Physical and cognitive rest is crucial in the acute phase of injury to allow the brain to heal. Depending on the severity of symptoms and individual circumstances, healthcare providers may recommend gradually resuming activities once symptoms improve.
In some cases, medication may be prescribed to manage specific symptoms such as headache, nausea, or sleep disturbances. Cognitive rehabilitation therapy, vestibular rehabilitation, and other forms of specialized therapy may also be recommended to address persistent symptoms and facilitate recovery.
It’s essential to follow the guidance of healthcare professionals and gradually return to normal activities, including work, school, and physical exercise, to minimize the risk of complications and ensure a safe and full recovery. If symptoms persist or worsen over time, further evaluation and monitoring may be necessary to address any underlying issues and support long-term recovery.
The knee is a complex joint that plays a crucial role in supporting the body’s weight and facilitating movement. Knee pain can be a common complaint and may arise from various causes, ranging from acute injuries to chronic conditions. Understanding the potential causes of knee pain, when to seek medical help, and available treatment options is essential for effective management.
Call the office or book an appointment online today.
Acute Injuries: These include ligament sprains or tears (such as ACL or MCL injuries), meniscus tears, fractures, dislocations, or patellar (kneecap) injuries. These injuries often occur due to sudden trauma or overuse during sports activities or accidents.
Osteoarthritis: This degenerative joint disease occurs when the cartilage that cushions the ends of the bones within the knee joint gradually wears away. Osteoarthritis can lead to pain, stiffness, swelling, and decreased mobility in the knee.
Rheumatoid Arthritis: An autoimmune condition that causes chronic inflammation of the joints, including the knee. Rheumatoid arthritis can result in pain, swelling, warmth, and deformity of the knee joint.
Patellofemoral Pain Syndrome (Runner’s Knee): This condition involves pain around or behind the kneecap, often aggravated by activities that involve bending the knee, such as running, squatting, or climbing stairs.
Bursitis: Inflammation of the bursae, small fluid-filled sacs that cushion the knee joint, can lead to pain, swelling, and tenderness around the knee.
Tendonitis: Inflammation of the tendons surrounding the knee, such as patellar tendonitis (jumper’s knee) or quadriceps tendonitis, can cause pain, stiffness, and difficulty with movement.
Overuse or Repetitive Strain: Activities that involve repetitive bending, kneeling, or squatting can strain the structures of the knee joint, leading to pain and discomfort.
You should seek medical attention for knee pain if:
Treatment for knee pain depends on the underlying cause and severity of the condition. It may include:
Rest and Activity Modification: Avoid activities that exacerbate knee pain and allow the joint to rest and heal.
Physical Therapy: Exercises to strengthen the muscles around the knee, improve flexibility, and restore range of motion.
Pain Management: Over-the-counter pain relievers, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), can help alleviate pain and inflammation.
RICE Therapy: Rest, ice, compression, and elevation can reduce swelling and pain associated with acute knee injuries.
Bracing or Splinting: Supportive braces or splints may be used to stabilize the knee joint and provide pain relief.
Corticosteroid Injections: Injections of corticosteroids into the knee joint can help reduce inflammation and relieve pain, especially for conditions like arthritis or bursitis.
Surgery: In severe cases or when conservative treatments fail, surgical interventions such as arthroscopy, ligament reconstruction, meniscus repair, or knee replacement may be necessary.
It’s essential to consult with a healthcare professional, such as an orthopedic specialist or sports medicine physician, for a thorough evaluation and personalized treatment plan tailored to your specific needs. Early intervention and appropriate management can help alleviate knee pain and prevent further complications, allowing you to maintain an active and healthy lifestyle.
A concussion is a type of traumatic brain injury (TBI) caused by a sudden jolt, blow, or bump to the head or body that results in the brain’s rapid movement within the skull. This movement can cause stretching and damage to brain cells and disrupt normal brain function temporarily. Concussions are often referred to as mild TBIs because they are usually not life-threatening, but they can have serious short-term and long-term effects on cognitive, physical, and emotional health. Our sports medicine program includes specialized care for athletes who have sustained concussions or head injuries. Our sports medicine physicians are trained in concussion evaluation and management protocols, including sideline assessment, symptom monitoring, neurocognitive testing, and gradual return-to-play protocols. We prioritize the safety and well-being of athletes with concussions, providing comprehensive care to support their recovery and minimize the long-term effects of head injuries.
Call the office or book an appointment online today.
What are the symptoms of concussion?
Symptoms of Concussion:
Headache or Pressure in the Head: The most common symptom of concussion is a headache, which may vary in intensity.
Dizziness or Balance Problems: Feeling dizzy, lightheaded, or unsteady on your feet is common after a concussion.
Nausea or Vomiting: Some individuals may experience nausea or vomiting after sustaining a concussion.
Confusion or Disorientation: Difficulty concentrating, feeling mentally foggy, or having trouble remembering events before or after the injury.
Sensitivity to Light or Noise: Increased sensitivity to light or noise, known as photophobia and phonophobia, respectively.
Visual Disturbances: Blurred or double vision, seeing stars, or difficulty focusing on objects.
Fatigue or Drowsiness: Feeling unusually tired, lethargic, or sleepy even after getting adequate rest.
Sleep Disturbances: Changes in sleep patterns, such as difficulty falling asleep, excessive sleepiness, or disrupted sleep.
Mood Changes: Irritability, mood swings, anxiety, depression, or emotional instability may occur following a concussion.
Memory Problems: Difficulty recalling recent events, difficulty concentrating, or feeling mentally sluggish.
When do seek medical Attention?
It’s essential to seek medical attention if you or someone else experiences any of the following symptoms after a head injury:
Deteriorating mental status (confusion, agitation, difficulty waking up) Loss of consciousness: Although not all concussions involve loss of consciousness, if it does occur, especially for an extended period, it can indicate a more severe brain injury.
Worsening symptoms: If symptoms such as headache, dizziness, confusion, or nausea worsen over time rather than improving, it could suggest an evolving brain injury.
Seizures: Seizures following a head injury can be a sign of a more severe brain injury and require immediate medical attention.
Persistent vomiting: Vomiting that continues or worsens after the initial injury may indicate increased intracranial pressure and should be evaluated promptly.
Unequal pupil size: Also known as anisocoria, a significant difference in the size of the pupils can be a sign of serious brain injury or other neurological problems.
Severe or worsening headache: While headaches are common after a concussion, if they are severe, persistent, or getting worse, it may indicate a more serious issue.
Weakness or numbness: Weakness or numbness, especially on one side of the body, can indicate damage to the brain or spinal cord and should be evaluated immediately.
Difficulty waking up: If someone has difficulty waking up or appears excessively drowsy after a head injury, it could indicate a more severe brain injury.
Confusion or agitation: Severe confusion, unusual behavior, or agitation following a head injury may be signs of a more severe brain injury.
Slurred speech: Difficulty speaking clearly, or slurred speech can be a sign of neurological impairment and should be evaluated promptly.
The primary treatment for concussion involves rest and avoiding activities that may exacerbate symptoms. Physical and cognitive rest is crucial in the acute phase of injury to allow the brain to heal. Depending on the severity of symptoms and individual circumstances, healthcare providers may recommend gradually resuming activities once symptoms improve.
In some cases, medication may be prescribed to manage specific symptoms such as headache, nausea, or sleep disturbances. Cognitive rehabilitation therapy, vestibular rehabilitation, and other forms of specialized therapy may also be recommended to address persistent symptoms and facilitate recovery.
It’s essential to follow the guidance of healthcare professionals and gradually return to normal activities, including work, school, and physical exercise, to minimize the risk of complications and ensure a safe and full recovery. If symptoms persist or worsen over time, further evaluation and monitoring may be necessary to address any underlying issues and support long-term recovery.
45 min 170 US dollars
InfusionZone illness Recovery therapy is specifically formulated to help you bounce back from any form of illness quickly and effectively. This carefully crafted blend contains a combination of essential nutrients to support your body’s natural healing processes and alleviate symptoms.
Our InfusionZone illness Recovery therapy is one of our selected favorites, trusted by many to aid in the recovery process and minimize symptoms. Whether you’re dealing with the flu, a cold, or any other illness, this therapy can provide the relief and support you need to get back on your feet quickly.
Experience the rejuvenating effects of InfusionZone illness Recovery therapy today and accelerate your path to wellness. Contact us to schedule your appointment and start feeling better soon.
The United States has over 3.5 million childhood sports related injuries reported yearly, which are concerning to parents. These injuries can range from minor sprains to more severe fractures, impacting a child’s physical activity and overall well-being. Recognizing the importance of specialized care for pediatric sports injuries, Healthzone MD Family and Sports Medicine Wellness Center offers comprehensive diagnosis and treatment for children facing such challenges.
Call the office or book an appointment online today.
What is pediatric sports medicine?
Pediatric sports medicine focuses on assessing, treating, and preventing injuries and illnesses related to physical activity in children and adolescents.
Why should my child see a pediatric sports medicine specialist?
Children have unique medical needs, and Healthzone MD sports medicine specialists are trained to understand and address these differences. They can recognize symptoms that may be difficult for children to communicate and are knowledgeable about growth plate injuries, common in growing children.
What conditions does a pediatric sports medicine specialist treat?
At Healthzone MD Family and Sports Medicine Wellness Center we treat a variety of sports-related injuries and conditions in children, including sprains, fractures, growth plate injuries, tendinitis, concussions, and more. They also provide guidance on nutrition and supplements, addressing concerns like the female athlete triad.
What should I expect from a pediatric sports medicine visit?
During the visit, your child’s symptoms and medical history will be reviewed, followed by a physical exam. The team may conduct a comprehensive functional evaluation to identify any biomechanical imbalances. Based on this assessment, a personalized treatment plan will be created, utilizing state-of-the-art equipment and technology for optimal care.
For pediatric sports medicine expertise, contact HealthZone MD Family and Sports Medicine Wellness Center or schedule an appointment online.
The Healthline MD Family and Sports Medicine Wellness Center Sports Medicine program offers comprehensive care for athletes of all ages and levels. Our program is designed to address the unique needs of athletes, optimizing athletic performance, preventing injuries, and promoting overall health and well-being in athletes of all ages and skill levels. Our clinic manages various aspects of sports-related injuries and conditions, including acute injuries such as sprains, strains, fractures, dislocations, and concussions, as well as chronic conditions like tendonitis, bursitis, stress fractures, and overuse injuries.
Call the office or book an appointment online today.
Sports medicine is a specialized field of healthcare that focuses on the prevention, diagnosis, treatment, and rehabilitation of injuries related to sports and exercise. It encompasses a multidisciplinary approach, involving physicians, orthopedic surgeons, physical therapists, athletic trainers, nutritionists, and other healthcare professionals who collaborate to optimize athletic performance, prevent injuries, and promote overall health and well-being in athletes of all ages and skill levels. Sports medicine physicians are trained to evaluate and diagnose these injuries, often using advanced diagnostic tools such as imaging studies (X-rays, MRI, CT scans) and physical examination techniques.
Once a diagnosis is made, sports medicine practitioners develop individualized treatment plans tailored to the athlete’s specific needs, goals, and level of activity. Treatment modalities may include non-surgical interventions such as rest, ice, compression, elevation (RICE), physical therapy, rehabilitative exercises, bracing, and medication management for pain and inflammation. In cases where surgery is necessary, sports medicine physicians work closely with orthopedic surgeons to coordinate surgical interventions and post-operative rehabilitation protocols.
In addition to injury treatment, sports medicine also emphasizes injury prevention strategies to reduce the risk of sports-related injuries and optimize athletic performance. This may involve educating athletes, coaches, and parents about proper warm-up and cool-down techniques, biomechanics, strength and conditioning exercises, flexibility training, nutrition, hydration, sleep hygiene, and sports safety guidelines. Sports medicine practitioners may also conduct pre-participation physical exams (PPEs) to assess an athlete’s overall health and fitness level before participating in sports activities.
Sports medicine is not limited to competitive athletes; it also serves individuals who engage in recreational sports and exercise for fitness and leisure. Sports medicine practitioners work with athletes of all ages and abilities, from children and adolescents to adults and seniors, across various sports and physical activities, including team sports, individual sports, endurance sports, and recreational activities.
Overall, sports medicine plays a crucial role in helping athletes stay healthy, recover from injuries, and perform at their best, whether they are competing at the highest level or simply staying active for health and enjoyment. By combining medical expertise, evidence-based practice, and a holistic approach to care, sports medicine professionals help athletes achieve their goals and maintain lifelong participation in sports and physical activity.
You should see a HealthZone MD Family and Sports Medicine Specialist if you experience any of the following:
Acute injuries: If you sustain an acute injury while participating in sports or physical activity, such as sprains, strains, fractures, dislocations, or concussions, a sports medicine specialist can assess the injury, provide an accurate diagnosis, and recommend appropriate treatment to help you recover safely and quickly.
Chronic or overuse injuries: If you have persistent pain or discomfort that develops gradually over time due to repetitive stress or overuse of certain muscles, tendons, or joints, a sports medicine specialist can evaluate the underlying cause of your symptoms, develop a personalized treatment plan, and implement strategies to prevent recurrence.
Performance enhancement: If you are an athlete looking to improve your athletic performance, prevent injuries, or optimize your training regimen, a sports medicine specialist can provide guidance on sports-specific conditioning, biomechanics, strength training, flexibility exercises, nutrition, hydration, and recovery strategies to help you reach your full potential.
Pre-participation physical exams (PPEs): If you are planning to participate in organized sports or physical activity, especially at the high school, college, or professional level, many leagues and organizations require athletes to undergo a pre-participation physical exam (PPE) to assess their overall health, fitness level, and readiness to participate safely.
Concussion management: If you experience a head injury or concussion while participating in sports or recreational activities, it is essential to seek medical attention from a sports medicine specialist who is trained in concussion management. They can evaluate your symptoms, monitor your recovery, and provide guidance on when it is safe to return to play.
Sports medicine procedures and treatments performed by HealthZone MD Family and Sports Medicine Specialist may include:
Evaluation and diagnosis: Sports medicine specialists use a variety of diagnostic tools and techniques, such as physical examination, imaging studies (X-rays, MRI, CT scans), and functional assessments, to accurately diagnose sports-related injuries and conditions.
Non-surgical interventions: Many sports injuries can be effectively treated with non-surgical approaches, such as rest, ice, compression, elevation (RICE), physical therapy, rehabilitative exercises, bracing, and medication management for pain and inflammation.
Surgical interventions: In cases where conservative treatments are not sufficient to address the injury or condition, sports medicine physicians may collaborate with orthopedic surgeons to perform surgical procedures, such as arthroscopic surgery, ligament reconstruction, tendon repair, or fracture fixation.
Rehabilitation: Following injury or surgery, HealthZone MD Family and Sports medicine specialists develop individualized rehabilitation programs to help athletes regain strength, mobility, flexibility, and function. Rehabilitation may involve supervised exercises, manual therapy techniques, neuromuscular re-education, proprioceptive training, and sport-specific functional training.
Injury prevention: HealthZone MD Family and Sports medicine specialists focus on implementing injury prevention strategies to reduce the risk of sports-related injuries, including proper warm-up and cool-down techniques, biomechanical assessments, strength and conditioning programs, flexibility training, nutritional counseling, hydration strategies, sleep hygiene, and sports safety education.
Overall, sports medicine plays a crucial role in helping athletes of all ages and abilities stay healthy, recover from injuries, and perform at their best. By combining medical expertise, evidence-based practice, and a multidisciplinary approach to care, sports medicine specialists help individuals achieve their athletic goals and maintain lifelong participation in sports and physical activity.
The Sports Nutrition and Wellness program at HealthZone MD Family and Sports Medicine Wellness Center is a comprehensive program designed to optimize the nutrition, health, and performance of athletes of all levels, from recreational enthusiasts to elite competitors. Our program integrates evidence-based nutrition strategies, personalized meal planning, supplementation guidance, and lifestyle interventions to support athletes in achieving their performance goals, enhancing recovery, and maintaining overall health and well-being. Here’s an overview of our Sports Nutrition and Wellness program:
Nutritional Assessment and Counseling: Every athlete undergoes a thorough nutritional assessment conducted by our registered dietitians or nutrition specialists to evaluate their dietary habits, nutritional status, energy needs, and performance goals. This assessment may include dietary intake analysis, body composition assessment, metabolic testing, and consideration of any specific dietary preferences, restrictions, or food intolerances.
Personalized Meal Planning: Based on the results of the nutritional assessment, personalized meal plans are developed to meet the individualized nutritional needs and goals of each athlete. These meal plans are tailored to optimize energy intake, macronutrient distribution (carbohydrates, protein, fat), micronutrient adequacy, hydration status, and timing of meals and snacks relative to training and competition schedules. Meal plans may also address specific performance objectives, such as muscle gain, weight management, endurance, or recovery.
Nutrition Education and Counseling: Athletes receive comprehensive nutrition education and counseling to enhance their understanding of the role of nutrition in optimizing performance, recovery, and overall health. Our nutrition experts provide guidance on topics such as macronutrients and micronutrients, hydration strategies, nutrient timing, fueling before, during, and after exercise, dietary supplements, portion control, grocery shopping, meal preparation, and dining out strategies.
Hydration Optimization: Proper hydration is critical for athletic performance, especially in hot and humid environments or during prolonged exercise sessions. Our Sports Nutrition and Wellness program includes guidance on optimal hydration strategies to maintain fluid balance, prevent dehydration, and minimize the risk of heat-related illnesses. Athletes learn how to monitor their fluid intake, assess hydration status, and implement strategies to stay adequately hydrated before, during, and after training and competition.
Supplementation Guidance: While a well-balanced diet should provide most of the nutrients needed for optimal performance and health, certain athletes may benefit from targeted supplementation to address specific nutritional deficiencies, support recovery, or enhance performance. Our nutrition experts provide evidence-based guidance on the safe and appropriate use of dietary supplements, including vitamins, minerals, amino acids, ergogenic aids, and sports nutrition products. Athletes learn how to navigate the supplement marketplace, evaluate product quality and safety, and avoid banned substances prohibited by anti-doping regulations.
Nutrition for Recovery and Injury Prevention: Proper nutrition plays a crucial role in supporting recovery from training and injury, reducing inflammation, promoting tissue repair, and preventing overtraining and injury. Our Sports Nutrition and Wellness program emphasizes the importance of post-exercise nutrition strategies to replenish glycogen stores, repair muscle damage, and support immune function. Athletes receive guidance on incorporating nutrient-rich foods, antioxidant-rich foods, and anti-inflammatory foods into their diet to support recovery and reduce the risk of injury.
Long-Term Health and Performance Optimization: In addition to supporting immediate performance goals, our Sports Nutrition and Wellness program focuses on promoting long-term health and performance optimization. Athletes learn how to adopt sustainable dietary habits, lifestyle behaviors, and mindset strategies to support their athletic endeavors while prioritizing overall health, well-being, and longevity. Our goal is to empower athletes with the knowledge, skills, and tools to fuel their bodies effectively, maximize their athletic potential, and thrive both on and off the field.
Overall, our Sports Nutrition and Wellness program at HealthZone MD Family and Sports Medicine Wellness Center provides athletes with the comprehensive support and guidance they need to optimize their nutrition, health, and performance. By integrating evidence-based nutrition strategies, personalized meal planning, hydration optimization, supplementation guidance, and injury prevention strategies, we help athletes achieve their performance goals, recover effectively, and maintain long-term health and well-being.
The Return-to-Sport Protocol program at HealthZone MD Family and Sports Medicine Wellness Center is specifically designed to guide athletes through a structured and comprehensive process of safely returning to their sport following injury or extended periods of inactivity. Our program focuses on restoring physical function, optimizing performance, reducing the risk of re-injury, and facilitating a smooth transition back to athletic participation. Here’s an overview of our Return-to-Sport Protocol program:
Initial Evaluation and Assessment: Every athlete undergoes a thorough initial evaluation and assessment by our experienced sports medicine team to determine the extent of their injury, assess their current physical condition, and identify any underlying factors that may affect their return to sport. This evaluation may include medical history review, physical examination, diagnostic imaging (if necessary), and functional testing.
Injury Rehabilitation and Treatment: Based on the findings of the initial assessment, a customized rehabilitation and treatment plan is developed to address the specific needs and goals of the athlete. Our multidisciplinary team of sports medicine specialists, physical therapists, athletic trainers, and other healthcare professionals collaborate to provide comprehensive care and support throughout the rehabilitation process. Treatment modalities may include manual therapy, therapeutic exercises, modalities (e.g., ultrasound, electrical stimulation), joint mobilizations, and therapeutic taping.
Progressive Rehabilitation Program: Our rehabilitation program follows a progressive and individualized approach, gradually increasing in intensity and complexity as the athlete progresses through different stages of recovery. The program focuses on restoring range of motion, strength, flexibility, endurance, balance, proprioception, and sport-specific skills relevant to the athlete’s sport and position. Each phase of the rehabilitation program is carefully monitored, and adjustments are made based on the athlete’s response to treatment and objective progress.
Functional and Performance Testing: Throughout the rehabilitation process, functional and performance testing is conducted to assess the athlete’s readiness to return to sport safely. Functional tests may include dynamic movement assessments, agility drills, balance tests, plyometric exercises, and sport-specific skill assessments. Performance testing may involve measures of strength, power, speed, endurance, and sport-specific performance metrics. These tests help to objectively evaluate the athlete’s physical function, identify any remaining deficits or asymmetries, and determine their readiness to progress to the next phase of rehabilitation.
Gradual Return-to-Sport Progression: Once the athlete has successfully completed the rehabilitation program and demonstrated sufficient physical function and performance capabilities, a gradual return-to-sport progression is initiated. This progression involves gradually reintroducing sport-specific activities, drills, and exercises in a controlled manner, starting with low-risk activities and gradually increasing the intensity, duration, and complexity of training. The athlete’s response to sport-specific movements and exercises is closely monitored, and adjustments are made as needed to minimize the risk of re-injury.
Education and Injury Prevention Strategies: Throughout the return-to-sport process, athletes receive education and guidance on injury prevention strategies, proper technique, biomechanics, training principles, recovery strategies, and lifestyle factors that may affect their performance and injury risk. Athletes are empowered with the knowledge and tools to maintain their physical health, optimize their performance, and minimize the risk of future injuries.
Follow-Up and Continued Support: Our sports medicine team provides ongoing follow-up care and support to athletes as they transition back to full athletic participation. Regular progress assessments, re-evaluations, and check-ins are conducted to monitor the athlete’s progress, address any concerns or setbacks, and make any necessary adjustments to their rehabilitation plan. Our goal is to ensure a successful return to sport, promote long-term athletic success, and support the athlete’s overall health and well-being.
Overall, HealthZone MD Family and Sports Medicine Wellness Center Return-to-Sport Protocol program is designed to facilitate a safe and successful return to athletic participation following injury, surgery, or extended periods of inactivity. By focusing on comprehensive rehabilitation, progressive training, functional performance testing, education, and ongoing support, we help athletes regain confidence, optimize their performance, and enjoy a fulfilling and successful return to sport.
Call the office or book an appointment online today.
The Performance Enhancement Program at HealthZone MD Family and Sports Medicine Wellness Center is designed to optimize athletic performance, prevent injuries, and promote overall wellness for athletes of all ages and skill levels. Our comprehensive program integrates evidence-based training principles, cutting-edge technology, and personalized coaching to help athletes reach their full potential and achieve their performance goals. Here are some key components of our Performance Enhancement Program:
Comprehensive Assessment: Every athlete undergoes a comprehensive assessment to evaluate their current fitness level, movement mechanics, strength, flexibility, agility, speed, power, and sport-specific skills. This assessment helps our team identify areas of strength and areas for improvement to develop an individualized performance enhancement plan.
Functional Movement Screening: We utilize functional movement screening tools to assess movement patterns, identify asymmetries, and detect movement dysfunctions that may predispose athletes to injury or limit performance. Based on the results of the screening, we design targeted interventions to address movement deficiencies and enhance functional movement patterns.
Strength and Conditioning: Our strength and conditioning programs are tailored to the specific needs and goals of each athlete, taking into account their sport, position, age, skill level, and injury history. We focus on improving muscular strength, power, endurance, and stability through progressive resistance training, plyometric exercises, agility drills, and functional movements.
Speed and Agility Training: Speed and agility are crucial components of athletic performance across various sports. Our program includes speed and agility training protocols designed to enhance acceleration, deceleration, change of direction, agility, and quickness. We utilize advanced training techniques, such as sprint drills, ladder drills, cone drills, and agility ladder exercises, to improve speed and agility performance.
Flexibility and Mobility Training: Optimal flexibility and mobility are essential for preventing injuries, improving movement efficiency, and enhancing athletic performance. We incorporate targeted stretching, dynamic mobility exercises, myofascial release techniques, and joint mobilizations to improve flexibility, joint range of motion, and tissue extensibility.
Sport-Specific Skill Development: Our program emphasizes sport-specific skill development to enhance technical proficiency, tactical awareness, and game intelligence in athletes. We provide specialized coaching and instruction in sport-specific skills, such as shooting, passing, dribbling, hitting, throwing, catching, and positional play, tailored to the requirements of each sport.
Injury Prevention Strategies: Injury prevention is a key focus of our Performance Enhancement Program. We implement evidence-based injury prevention strategies, such as neuromuscular training, balance training, proprioceptive training, and corrective exercises, to reduce the risk of common sports-related injuries, such as ACL tears, ankle sprains, and shoulder injuries.
Nutrition and Hydration Guidance: Proper nutrition and hydration are essential for supporting athletic performance, recovery, and overall health. Our program includes nutrition and hydration guidance provided by registered dietitians and sports nutrition experts. We educate athletes on optimal fueling strategies, hydration practices, nutrient timing, and supplementation to maximize performance and optimize recovery.
Mental Skills Training: Mental toughness, focus, confidence, and resilience are critical for success in sports. Our program incorporates mental skills training techniques, such as goal setting, visualization, mindfulness, relaxation techniques, and performance psychology strategies, to enhance mental toughness and psychological resilience in athletes.
Monitoring and Evaluation: We utilize advanced monitoring and evaluation tools, such as performance testing, biomechanical analysis, wearable technology, and athlete monitoring systems, to track progress, monitor performance metrics, and adjust training interventions as needed. Regular progress assessments and performance evaluations help athletes stay on track toward their goals and make data-driven decisions to optimize their training program.
Overall, our Performance Enhancement Program is designed to empower athletes to unlock their full potential, improve athletic performance, reduce the risk of injury, and achieve peak performance in their sport. Whether you’re an elite athlete striving for podium finishes or a recreational athlete looking to enhance your skills and fitness level, our experienced team is here to support you on your journey to athletic excellence and success.
Call the office or book an appointment online today.
The Rehabilitation and Physical Therapy Program at HealthZone MD Family and Sports Medicine Wellness Center is dedicated to helping individuals recover from injuries, surgeries, and chronic conditions while maximizing their functional abilities and quality of life. Our program is led by a team of experienced physical therapists, rehabilitation specialists, and sports medicine professionals who are committed to providing personalized care tailored to each patient’s unique needs and goals. Here are some key components of our Rehabilitation and Physical Therapy Program:
Comprehensive Evaluation: Every patient undergoes a comprehensive evaluation to assess their musculoskeletal function, mobility, strength, flexibility, and functional limitations. This evaluation helps our team develop an individualized treatment plan based on the patient’s specific condition, goals, and preferences.
Evidence-Based Treatment Approaches: Our rehabilitation and physical therapy interventions are based on the latest evidence-based practices and guidelines. We utilize a wide range of treatment modalities, techniques, and therapeutic exercises to address pain, restore mobility, improve strength, and enhance overall function.
Manual Therapy: Manual therapy techniques, such as joint mobilization, soft tissue mobilization, and myofascial release, are often incorporated into treatment to improve joint mobility, reduce pain, and optimize tissue healing. These hands-on techniques are performed by skilled therapists to target areas of tightness, stiffness, or dysfunction.
Therapeutic Exercise Programs: Customized therapeutic exercise programs are designed to strengthen muscles, improve flexibility, enhance balance, and restore functional movement patterns. These programs may include exercises targeting specific muscle groups, proprioceptive training, balance exercises, and functional activities tailored to the patient’s goals and functional abilities.
Modalities and Therapeutic Agents: We offer a variety of modalities and therapeutic agents to complement therapeutic exercise and manual therapy interventions. These may include electrical stimulation, ultrasound, heat therapy, cold therapy, traction, and laser therapy, among others, to reduce pain, inflammation, and muscle spasm.
Sports-Specific Rehabilitation: For athletes recovering from sports injuries or orthopedic surgeries, our program provides sports-specific rehabilitation tailored to the demands of their sport and position. This may include sport-specific exercises, functional training, agility drills, plyometric exercises, and sport-specific conditioning to facilitate safe return to play.
Post-Surgical Rehabilitation: We specialize in post-surgical rehabilitation for patients undergoing orthopedic surgeries, such as joint replacements, ligament reconstructions, tendon repairs, and arthroscopic procedures. Our team works closely with surgeons to develop comprehensive rehabilitation protocols aimed at optimizing surgical outcomes and facilitating full recovery.
Pain Management Strategies: We employ various pain management strategies to help patients manage acute and chronic pain throughout the rehabilitation process. This may include education on pain neuroscience, pacing strategies, relaxation techniques, ergonomic modifications, and activity modification strategies to promote pain relief and improve function.
Patient Education and Home Exercise Programs: Patient education is an integral part of our Rehabilitation and Physical Therapy Program. We empower patients with the knowledge and skills they need to manage their condition, prevent re-injury, and maintain long-term musculoskeletal health. Home exercise programs are provided to reinforce in-clinic interventions and promote continuity of care.
Functional Rehabilitation and Return to Activity: Our ultimate goal is to help patients achieve their optimal level of function and safely return to their desired activities, whether it’s sports, work, or daily life. We focus on improving functional capacity, movement efficiency, and performance to support a successful return to activity with confidence and independence.
Overall, our Rehabilitation and Physical Therapy Program is dedicated to delivering high-quality, patient-centered care that addresses the unique needs and goals of each individual. Whether you’re recovering from an injury, surgery, or chronic condition, our experienced team is here to support you every step of the way on your journey to recovery and improved musculoskeletal health.
The Sports Injury Clinic Prevention Program at HealthZone MD Family and Sports Medicine Wellness Center is designed to reduce the risk of sports-related injuries among athletes of all ages and skill levels. Through a comprehensive approach that combines education, training, and proactive measures, our program aims to promote safe participation in sports activities while maximizing athletic performance and overall well-being. Here are some key components of our Sports Injury Clinic Prevention Program:
Pre-Participation Screening: Before participating in sports activities, athletes undergo thorough pre-participation screenings conducted by our team of sports medicine specialists. These screenings assess the athlete’s medical history, current health status, physical fitness, and any pre-existing conditions that may predispose them to injuries.
Individualized Risk Assessment: Each athlete receives an individualized risk assessment to identify specific factors that may increase their risk of sports-related injuries. This assessment may include biomechanical evaluations, movement assessments, and functional testing to detect areas of weakness, imbalance, or dysfunction.
Education and Training: Athletes, coaches, and parents are educated about the importance of injury prevention and provided with training on proper warm-up techniques, cool-down exercises, stretching routines, and injury prevention strategies. This includes guidance on proper form, technique, equipment use, and nutrition to support optimal performance and reduce injury risk.
Strength and Conditioning Programs: Our Sports Injury Clinic offers strength and conditioning programs tailored to the individual needs and goals of each athlete. These programs focus on building strength, flexibility, agility, and endurance while addressing any biomechanical imbalances or weaknesses that may contribute to injury risk.
Sports-Specific Training: Athletes receive sports-specific training designed to enhance their skills, improve their performance, and reduce the risk of injuries associated with their chosen sport. This may include sport-specific drills, exercises, and conditioning routines tailored to the demands of the sport and the athlete’s position or role.
Injury Prevention Workshops: Periodic injury prevention workshops are conducted to educate athletes, coaches, and parents about common sports-related injuries, risk factors, warning signs, and preventive measures. These workshops cover topics such as concussion management, heat illness prevention, overuse injury prevention, and injury rehabilitation.
Injury Surveillance and Monitoring: Our Sports Injury Clinic conducts ongoing surveillance and monitoring of sports-related injuries to identify trends, patterns, and risk factors within our athlete population. This data-driven approach allows us to implement targeted interventions and adjust our prevention strategies accordingly.
Collaboration with Coaches and Athletic Trainers: We collaborate closely with coaches, athletic trainers, and other members of the athlete’s support team to ensure a coordinated approach to injury prevention. This includes regular communication, injury reporting, and collaborative decision-making to optimize athlete safety and performance.
Research and Innovation: Our Sports Injury Clinic is actively involved in research and innovation initiatives aimed at advancing the field of sports injury prevention. Through ongoing research studies, clinical trials, and collaborative partnerships, we strive to develop and implement cutting-edge strategies to reduce the incidence and severity of sports-related injuries.
Community Outreach and Engagement: HealthZone MD Family and Sports Medicine Wellness Center engages with the local community through outreach programs, educational events, and partnerships with schools, youth sports organizations, and recreational leagues. By raising awareness about sports injury prevention and promoting safe participation in sports, we aim to empower athletes of all ages to enjoy the benefits of physical activity while minimizing the risk of injuries.
Overall, our Sports Injury Clinic Prevention Program is committed to providing comprehensive, evidence-based care to help athletes stay healthy, perform at their best, and achieve their athletic goals safely and effectively. Through a combination of education, training, and proactive interventions, we strive to create a culture of safety, resilience, and excellence in sports.
Foot pain can be caused by a variety of factors, ranging from overuse injuries to underlying medical conditions. Understanding the potential causes of foot pain, when to seek medical attention, and available treatment options is essential for effective management.
Call the office or book an appointment online today.
Plantar Fasciitis: Inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot, often due to overuse, poor footwear, or biomechanical issues.
Achilles Tendinitis: Inflammation of the Achilles tendon, which connects the calf muscles to the heel bone, commonly caused by repetitive stress or overuse.
Metatarsalgia: Pain and inflammation in the ball of the foot, often associated with activities that involve running, jumping, or wearing high heels.
Foot Sprains: Stretching or tearing of the ligaments in the foot, typically resulting from trauma or sudden twisting movements.
Stress Fractures: Hairline cracks in the bones of the foot, commonly seen in athletes or individuals who engage in high-impact activities.
Bunions: Bony protrusions that develop at the base of the big toe, often due to genetics, improper footwear, or structural abnormalities.
Neuromas: Thickening of the tissue around a nerve in the foot, leading to pain, tingling, or numbness, commonly associated with wearing tight shoes.
Arthritis: Conditions like osteoarthritis or rheumatoid arthritis can affect the joints of the foot, resulting in pain, stiffness, and decreased mobility.
You should seek medical attention for foot pain if:
Treatment for foot pain depends on the underlying cause and severity of the condition. It may include:
Rest and Immobilization: Avoiding activities that exacerbate foot pain and using supportive devices such as orthotic inserts, braces, or splints to alleviate pressure on the affected area.
Ice and Elevation: Applying ice packs to the affected foot and elevating it above heart level can help reduce swelling and alleviate pain.
Pain Management: Over-the-counter pain relievers, such as acetaminophen or NSAIDs, can help alleviate pain and inflammation.
Physical Therapy: Exercises to strengthen the muscles of the foot, improve flexibility, and correct biomechanical issues contributing to foot pain.
Orthotic Devices: Custom-made shoe inserts or orthotic devices can provide support and stability to the foot and correct structural abnormalities.
Corticosteroid Injections: Injections of corticosteroids into the affected area can help reduce inflammation and relieve pain, especially for conditions like plantar fasciitis or arthritis.
Surgery: In severe cases or when conservative treatments fail, surgical interventions such as bunionectomy, tendon repair, or joint fusion may be necessary.
It’s important to consult with a healthcare professional, such as a podiatrist or orthopedic specialist, for a thorough evaluation and personalized treatment plan tailored to your specific needs. Early intervention and appropriate management can help alleviate foot pain, promote healing, and prevent further complications, allowing you to resume normal activities with minimal discomfort.
Ankle pain can stem from various causes, ranging from acute injuries to chronic conditions. Understanding the potential causes of ankle pain, when to seek medical help, and available treatment options is essential for effective management.
Call the office or book an appointment online today.
Causes of Ankle Sprain Include:
Sprains and Strains: One of the most common causes of ankle pain is a sprain, which occurs when the ligaments that support the ankle stretch or tear. Ankle sprains often result from twisting or rolling the ankle during physical activity. Strains involve stretching or tearing of the muscles or tendons around the ankle.
Fractures: Ankle fractures can occur when there is a break in one or more of the bones that make up the ankle joint, such as the tibia, fibula, or talus. Fractures may result from trauma, falls, or repetitive stress.
Tendonitis: Inflammation of the tendons around the ankle, such as Achilles tendonitis or peroneal tendonitis, can cause pain, swelling, and difficulty with movement. Tendonitis often develops due to overuse, repetitive strain, or sudden increases in activity.
Arthritis: Conditions like osteoarthritis or rheumatoid arthritis can affect the joints of the ankle, leading to pain, stiffness, swelling, and decreased mobility. Arthritis may develop as a result of age-related wear and tear, autoimmune disorders, or previous injuries.
Tarsal Tunnel Syndrome: Similar to carpal tunnel syndrome in the wrist, tarsal tunnel syndrome involves compression of the posterior tibial nerve as it passes through the tarsal tunnel in the ankle. This can cause pain, tingling, numbness, or weakness in the foot and ankle.
Bursitis: Inflammation of the bursae, small fluid-filled sacs that cushion the ankle joint, can result from overuse, repetitive motion, or trauma. Bursitis can lead to pain, swelling, and tenderness around the ankle.
Stress Fractures: Tiny cracks in the bones of the ankle, known as stress fractures, can develop over time due to repetitive stress or overuse. Athletes who engage in high-impact activities like running or jumping are particularly susceptible to stress fractures.
You should seek medical attention for ankle pain if:
Treatment for ankle pain depends on the underlying cause and severity of the condition. It may include:
Rest and Immobilization: Avoiding weight-bearing activities and using supportive devices like crutches, braces, or splints to stabilize the ankle and promote healing.
Ice and Elevation: Applying ice packs and elevating the affected ankle above heart level can help reduce swelling and alleviate pain.
Compression: Using compression bandages or wraps around the ankle can provide support and reduce swelling.
Physical Therapy: Exercises to strengthen the muscles around the ankle, improve flexibility, and restore range of motion.
Pain Management: Over-the-counter pain relievers, such as acetaminophen or NSAIDs, can help alleviate pain and inflammation.
Corticosteroid Injections: Injections of corticosteroids into the ankle joint can help reduce inflammation and relieve pain, especially for conditions like arthritis or tendonitis.
Surgery: In severe cases or when conservative treatments fail, surgical interventions such as ankle arthroscopy, ligament repair, or ankle fusion may be necessary.
It’s crucial to consult with a healthcare professional, such as an orthopedic specialist or sports medicine physician, for a thorough evaluation and personalized treatment plan tailored to your specific needs. Early intervention and appropriate management can help alleviate ankle pain, promote healing, and prevent further complications, allowing you to return to your usual activities with minimal discomfort.
The hip is a ball-and-socket joint that connects the thigh bone (femur) to the pelvis. It plays a crucial role in supporting the body’s weight, facilitating movement, and providing stability during various activities such as walking, running, and jumping. Like any other joint, the hip is susceptible to pain and discomfort, which can arise from a variety of causes.
Call the office or book an appointment online today.
Common causes of hip pain include:
Osteoarthritis: This is the most common form of arthritis, often occurring in older adults due to wear and tear of the hip joint over time. It causes the cartilage that cushions the hip joint to break down, leading to pain, stiffness, and decreased range of motion.
Hip Fractures: Fractures of the hip bone, particularly the femoral neck or the upper part of the femur, can occur due to trauma or falls, especially in older adults with weakened bones (osteoporosis). Hip fractures cause severe pain, swelling, and difficulty bearing weight on the affected leg.
Bursitis: Inflammation of the bursae, small fluid-filled sacs that cushion and lubricate the hip joint, can cause pain and tenderness in the outer part of the hip. Hip bursitis often occurs due to repetitive movements or overuse of the hip joint.
Tendonitis: Inflammation of the tendons, which attach muscles to bones, can occur in the hip area, causing pain and stiffness. Hip tendonitis is commonly seen in athletes or individuals who perform repetitive movements that strain the hip muscles and tendons.
Hip Labral Tears: Tears or damage to the labrum, a ring of cartilage that lines the rim of the hip socket, can occur due to trauma, repetitive movements, or structural abnormalities of the hip joint. Labral tears cause pain, clicking sensations, and limited hip mobility.
Muscle Strains: Strains or tears of the muscles surrounding the hip joint, such as the hip flexors or gluteal muscles, can result from sudden movements, overuse, or improper stretching techniques.
Hip Impingement: Also known as femoroacetabular impingement (FAI), hip impingement occurs when there is abnormal contact between the ball of the femur and the hip socket, leading to pain and potential damage to the joint structures.
Hip pain can significantly impact daily life, but with proper diagnosis and treatment, many individuals can find relief and regain function. It’s essential to consult with a healthcare professional for an accurate diagnosis and tailored treatment plan to address the underlying cause of hip pain effectively. Early intervention can help alleviate symptoms and prevent further complications, allowing individuals to resume their normal activities with reduced discomfort.
The elbow is a complex joint that connects the upper arm bone (humerus) to the two forearm bones (radius and ulna). It is responsible for the bending (flexion) and straightening (extension) of the arm, as well as rotational movements of the forearm. The elbow joint also allows for the pronation and supination of the forearm, which are movements that rotate the palm up or down. Several structures within and around the elbow joint can be sources of pain and discomfort and leading to elbow pain.
Call the office or book an appointment online today.
Elbow pain Q & A
Tennis elbow (lateral epicondylitis): This condition involves inflammation or degeneration of the tendons on the outside of the elbow, typically due to repetitive wrist and arm motions, such as those used in tennis or other sports, manual labor, or activities like typing.
Golfer’s elbow (medial epicondylitis): Similar to tennis elbow, golfer’s elbow involves inflammation or degeneration of the tendons on the inside of the elbow. It is often caused by repetitive wrist and forearm movements, such as those used in golf, throwing, or lifting.
Elbow sprains or strains: Overstretching or tearing of the ligaments or muscles around the elbow joint can occur due to sudden impact, trauma, or repetitive motions, leading to pain, swelling, and instability.
Bursitis: Inflammation of the bursa, fluid-filled sacs that cushion the joints, can develop around the elbow due to repetitive movements, trauma, or prolonged pressure, resulting in pain, swelling, and limited range of motion.
Olecranon bursitis: This condition involves inflammation of the bursa located at the tip of the elbow (olecranon), often caused by trauma, prolonged pressure, or infection, leading to pain, swelling, and tenderness at the back of the elbow.
Elbow arthritis: Degenerative changes or inflammation of the elbow joint due to conditions such as osteoarthritis or rheumatoid arthritis can cause pain, stiffness, and decreased range of motion.
Fractures or dislocations: Traumatic events, such as falls or direct blows to the elbow, can result in fractures (broken bones) or dislocations (when the bones are forced out of their normal position), causing severe pain, swelling, and difficulty moving the elbow.
Rest: Avoiding activities that worsen pain and resting the elbow joint can help promote healing.
Ice or heat therapy: Applying ice packs or heating pads to the affected area can help reduce inflammation and alleviate pain.
Pain medications: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or acetaminophen may help relieve pain and reduce inflammation.
Physical therapy: Specific exercises and stretches can help strengthen the muscles surrounding the elbow joint, improve flexibility, and reduce pain.
Immobilization: Using a splint, brace, or sling to immobilize the elbow joint may be necessary for certain injuries or conditions to allow for healing.
Corticosteroid injections: Injections of corticosteroids into the elbow joint can help reduce inflammation and alleviate pain, particularly for conditions such as tennis elbow or bursitis.
Occupational therapy: Occupational therapists can provide customized strategies and exercises to help improve elbow function and reduce pain, particularly for activities of daily living or work-related tasks.
In some cases, surgical intervention may be necessary to repair damaged tissues, remove loose bodies, or address underlying structural issues contributing to elbow pain. It’s essential to consult with a healthcare professional for a proper diagnosis and personalized treatment plan tailored to your specific condition and needs. Delaying treatment or ignoring persistent elbow pain may lead to further complications and long-term disability.
The shoulder is a highly mobile joint consisting of three bones: the humerus (upper arm bone), the scapula (shoulder blade), and the clavicle (collarbone). It is surrounded by a complex network of muscles, tendons, ligaments, and other soft tissues that work together to provide a wide range of motion and stability to the arm as a result it is prone to discomfort. Shoulder pain can arise from various underlying causes, ranging from minor strains to more serious conditions.
Call the office or book an appointment online today.
Rotator Cuff Injuries: The rotator cuff is a group of muscles and tendons that help stabilize the shoulder joint and facilitate movement. Injuries to the rotator cuff, such as tears or strains, are common causes of shoulder pain. These injuries can occur due to overuse, trauma, or degenerative changes associated with aging.
Frozen Shoulder (Adhesive Capsulitis): Frozen shoulder is a condition characterized by stiffness and pain in the shoulder joint, often accompanied by a gradual loss of motion. It typically develops over time and can be triggered by injury, surgery, or underlying medical conditions such as diabetes or thyroid disorders.
Labral Tears: The labrum is a ring of cartilage that surrounds the socket of the shoulder joint, providing stability and cushioning. Tears or damage to the labrum can occur due to trauma, repetitive overhead activities, or degenerative changes, leading to pain, instability, and a sensation of catching or locking in the shoulder.
Shoulder Arthritis: Arthritis of the shoulder joint can result from wear and tear (osteoarthritis), inflammation (rheumatoid arthritis), or other underlying conditions. It can cause pain, stiffness, swelling, and limited range of motion in the shoulder.
Bursitis: Bursitis is inflammation of the bursa, small fluid-filled sacs that cushion and lubricate the shoulder joint. It can develop due to overuse, trauma, or underlying conditions such as rotator cuff tears or arthritis, resulting in pain, swelling, and tenderness in the shoulder region.
Shoulder Dislocation or Instability: Shoulder dislocation occurs when the ball of the upper arm bone (humerus) slips out of the shoulder socket (glenoid). It can result from trauma or repetitive overhead motions and may cause severe pain, swelling, and instability. Recurrent dislocations or feelings of shoulder “looseness” may indicate shoulder instability.
Fractures or Trauma: Broken bones or other injuries to the shoulder, such as fractures of the collarbone (clavicle) or shoulder blade (scapula), can cause acute pain and dysfunction.
Referred Pain: Sometimes, pain perceived in the shoulder may originate from another source, such as the neck, spine, or organs like the heart or gallbladder.
Rest and Activity Modification: Avoiding activities that exacerbate the pain and modifying movements to reduce strain on the shoulder joint.
Physical Therapy: Exercises to improve strength, flexibility, and range of motion, as well as techniques to correct posture and movement mechanics.
Medications: Over-the-counter pain relievers, anti-inflammatory drugs, or muscle relaxants to alleviate pain and inflammation.
Steroid Injections: Corticosteroids injected into the shoulder joint or surrounding tissues to reduce inflammation and pain.
Heat or Cold Therapy: Applying heat packs or cold compresses to the affected area to help alleviate pain and promote healing.
Bracing or Immobilization: Using a sling, brace, or other supportive devices to stabilize the shoulder and facilitate healing, especially after injury or surgery.
Surgery: In cases of severe injury, instability, or irreparable damage to the shoulder joint, surgical intervention may be necessary to repair torn tissues, remove damaged structures, or replace the joint.
It’s essential to consult with a healthcare professional for an accurate diagnosis and appropriate management of shoulder pain to prevent further complications and optimize recovery.
Back pain is a prevalent condition that can range from a dull, constant ache to sudden, sharp pain. It can affect people of all ages and is one of the leading causes of disability worldwide. Back pain can originate from various structures in the spine, including muscles, ligaments, bones, discs, and nerves.
Call the office or book an appointment online today.
What causes Back pain?
Various factors can contribute to back pain, including:
Treatment for back pain depends on the underlying cause and severity of the symptoms. It may include:
Pain Management: Over-the-counter pain relievers like acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) can help alleviate mild to moderate back pain. Stronger medications or muscle relaxants may be prescribed for severe pain.
Physical Therapy: Targeted exercises and stretches can improve flexibility, strengthen the muscles supporting the spine, and promote proper posture.
Heat and Cold Therapy: Applying heat or cold packs to the affected area can help reduce inflammation and alleviate muscle spasms.
Manual Therapy: Techniques like Osteopathic Manipulation Technique, chiropractic adjustment, massage therapy, or acupuncture may provide relief by realigning the spine, releasing tension, and improving blood flow.
Injections: Corticosteroid injections directly into the affected area can temporarily reduce inflammation and alleviate pain.
Lifestyle Modifications: Avoiding activities that exacerbate the pain, maintaining a healthy weight, practicing good posture, and using proper body mechanics when lifting heavy objects can help prevent further strain on the back.
Surgery: In cases of severe or persistent back pain caused by spinal abnormalities like herniated discs or spinal stenosis, surgical intervention may be necessary to alleviate pressure on the nerves or stabilize the spine. However, surgery is typically considered a last resort when conservative treatments have failed to provide relief. It’s essential to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan tailored to your specific condition and needs.
Neck pain can arise from various causes, and while many cases resolve on their own with rest and self-care, some may require medical attention. Overall, early intervention and appropriate management can help alleviate neck pain and improve function, allowing individuals to resume their daily activities with minimal discomfort. It’s important to consult with a healthcare professional if you experience persistent or severe neck pain, especially if it’s accompanied by other symptoms such as weakness, numbness, tingling, or radiating pain into the arms or hands. A thorough evaluation can help determine the underlying cause of the neck pain and guide appropriate treatment.
Call the office or book an appointment online today.
What causes Neck Pain? Causes of neck pain includes:
Muscle Strain: Overuse, poor posture, or sudden movements can strain the muscles in the neck, leading to pain and stiffness.
Poor Posture: Maintaining improper posture while sitting, standing, or sleeping can put added stress on the neck muscles and joints.
Neck Injuries: Trauma from accidents, falls, or sports injuries can cause acute neck pain, such as whiplash.
Herniated Discs: Discs between the vertebrae may herniate or bulge out of place, pressing on nearby nerves and causing pain.
Degenerative Conditions: Arthritis, spinal stenosis, or degenerative disc disease can lead to chronic neck pain.
Poor Ergonomics: Prolonged periods of poor posture, such as hunching over a computer, can strain the neck.
Stress and Tension: Emotional stress and tension can cause muscle tightness and stiffness in the neck and shoulders.
Medical Conditions: Certain medical conditions like fibromyalgia, osteoporosis, or infections of the spine can cause neck pain.
Tumors: Tumors or growths in the cervical spine or surrounding tissues can lead to neck pain.
You should consider seeking medical help for neck pain if:
Treatment for neck pain depends on the underlying cause and severity of symptoms. Some common treatment options include:
Rest and Activity Modification: Avoid activities that exacerbate neck pain and practice good posture.
Pain Medications: Over-the-counter pain relievers like acetaminophen or NSAIDs may help alleviate pain and inflammation.
Physical Therapy: Stretching and strengthening exercises, as well as manual therapy techniques, can improve neck muscle strength and flexibility.
Heat and Cold Therapy: Applying heat or cold packs to the neck may help reduce pain and inflammation.
Medications: Muscle relaxants or prescription pain medications may be prescribed for severe neck pain.
Injections: Corticosteroid injections into the affected area can help reduce inflammation and pain.
Bracing or Collars: In some cases, wearing a cervical collar or brace may provide support and immobilization to the neck.
Alternative Therapies: Techniques such as acupuncture, chiropractic manipulation, or massage therapy may provide relief for some individuals.
Surgery: In rare cases where conservative treatments fail to provide relief, surgery may be recommended to address underlying structural issues.
It’s essential to consult with a healthcare professional for a proper diagnosis and individualized treatment plan tailored to your specific needs and condition. Early intervention and appropriate management can help alleviate neck pain and prevent potential complications.
Call the office or book an appointment online today.
45 min 150 US dollars
Our highly sought-after “Pregnancy” drip is meticulously crafted to provide essential hydration and effective relief from nausea tailored specifically for expectant mothers. Comprising 1 liter of normal saline infused with an intravenous Zofran, a potent anti-nausea medication, this drip ensures optimal hydration and swift alleviation of discomfort. Notably, the hydration is absorbed at an impressive rate of 100%, delivering immediate relief within just 15 minutes.
Administered in our state-of-the-art facility, this infusion guarantees a safe and comfortable environment for pregnant mothers. Prior to and following the infusion, each expectant mother undergoes a comprehensive evaluation by a skilled medical provider. This personalized approach ensures the utmost safety and well-being throughout the entire process, offering peace of mind and reassurance to both the mother and her loved ones.
Experience the unparalleled comfort and support of our Pregnancy drip as you embark on the beautiful journey of pregnancy with confidence and tranquility.
45 min 200 US dollars
Our tailored blend of respiratory vitamins, Zinc, and anti-inflammatory agents is crafted to alleviate upper respiratory pressure, combat seasonal allergies, and ease symptoms of the common cold. Designed to promote respiratory health and provide relief, this infusion is your solution to breathing easier and feeling better. Say goodbye to discomfort and hello to wellness with our Respiratory Support IV Therapy.
45 min 170 US dollars
Combat upper respiratory pressure, seasonal allergies, and the common cold with our customized blend of respiratory vitamins, Zinc, and an anti-inflammatory agent. This specialized infusion is designed to alleviate discomfort and promote respiratory wellness, providing targeted relief for your symptoms. Say goodbye to congestion and hello to easier breathing with our InfusionZone Respiratory Relief IV Therapy.
45 min 200 US dollars
Introducing our Everyday Hydration Therapy
Looking for a simple yet effective way to replenish your body’s fluids and electrolytes? Our Everyday Hydration Therapy is your go-to solution.
Whether you’re feeling dehydrated after a workout, a long day at work, or simply need a boost of hydration to feel your best, our Everyday Hydration Therapy is the perfect solution.
45 min 130 US dollars
Need a boost of fluids after a marathon, long flight, dehydration, headache, or viral illness? This is your everyday go to saline infusion. 100% cellular absorption guaranteed. Consider our popular add on anti- nausea Zofran or powerful antioxidant glutathione Iv push.
Hangover fix
45 min 170 US dollars
Introducing our InfusionZone Hangover Fix Therapy
Had a bit too much fun last night? We’ve got just what you need to bounce back and feel like yourself again. Our InfusionZone Hangover Fix Therapy is specifically formulated to help alleviate the symptoms of a hangover and get you back on your feet in no time.
Whether you’re dealing with a pounding headache, upset stomach, or overall fatigue, our InfusionZone Hangover Fix Therapy is here to provide the relief you need. Say goodbye to the effects of last night and hello to a fresh start with our rejuvenating drip.
Don’t let a hangover ruin your day – schedule your InfusionZone Hangover Fix Therapy today and get back to feeling your best in no time. Contact us to book your appointment and start your road to recovery.
45 min 200 US dollars
Are you looking for a natural way to strengthen your immune system and ward off illness? Our Immune Boost Therapy is designed to give your body the extra support it needs to fight off viruses and stay healthy, especially during cold and flu season.
Key Ingredients:
Our Immune Boost Therapy is the perfect solution for anyone looking to give their immune system a much-needed boost. Whether you’re dealing with the common cold, flu, stomach bug, or other viral illnesses, this drip is packed with essential nutrients to help your body defend itself and recover more quickly.
45 min 200 US dollars
Experience the Ultimate Replenishment with Myers’ Cocktail IV Infusion Therapy.
Myers’ Cocktail is a renowned intravenous nutrient therapy named after Dr. John Myers, who pioneered the use of intravenous vitamins and minerals for health and wellness. This powerful blend of vitamins and minerals is designed to replenish essential nutrients, support immune function, and promote overall well-being.
Ready to experience the rejuvenating benefits of Myers’ Cocktail IV Infusion Therapy? Contact us today to schedule your appointment and take the first step towards enhanced vitality and well-being. Our dedicated team is here to support you on your journey to optimal health and wellness.
At HealthZone MD Family and Sports Medicine Wellness Center, we prioritize preventive care and offer comprehensive screenings and health assessments to proactively monitor our patients’ health and identify any potential issues early on. Our preventive screenings and health assessments are designed to provide a thorough evaluation of various aspects of our patients’ health, allowing us to detect risk factors, prevent diseases, and promote overall wellness. Here’s an overview of the preventive screenings and health assessments we offer:
Routine Physical Examinations:
Health Risk Assessments:
Laboratory Testing:
Cancer Screenings:
Cardiovascular Assessments:
Bone Health Screenings:
Immunizations and Vaccinations:
Health Education and Counseling:
At HealthZone MD Family and Sports Medicine Wellness Center, we believe that preventive care is essential for maintaining optimal health and well-being. Our preventive screenings and health assessments are designed to identify health risks early, intervene proactively, and support our patients in achieving their health goals. Schedule a preventive care visit with us today to take proactive steps toward safeguarding your health and enjoying a lifetime of wellness.
At HealthZone MD Family and Sports Medicine Wellness Center, we understand the importance of skin health and rejuvenation for both aesthetic purposes and overall well-being. In collaboration dermatologist specialist we offer a comprehensive approach to skin care combines medical expertise with advanced technologies and personalized treatment plans to help our patients achieve healthy, radiant skin. Here’s an overview of the skin health and rejuvenation services we offer:
Medical Skin Assessments:
Customized Treatment Plans:
Advanced Skincare Products:
Cosmetic Procedures:
Acne Treatment:
Anti-Aging Therapies:
Sun Damage Repair:
At HealthZone MD Family and Sports Medicine Wellness Center, we are committed to helping our patients achieve healthy, vibrant skin at every stage of life. Whether you’re looking to address specific skin concerns, enhance your natural beauty, or maintain youthful-looking skin, our experienced team is here to provide personalized care and guidance. Schedule a consultation with us today to learn more about our skin health and rejuvenation services and take the first step toward achieving your skincare goals.
At HealthZone MD Family and Sports Medicine Wellness Center, we understand the importance of sexual health and fertility for overall well-being and quality of life. That’s why we offer comprehensive sexual health and fertility support services to address a wide range of concerns and needs. Our team of experienced healthcare professionals is dedicated to providing compassionate, personalized care to help individuals and couples optimize their sexual health and achieve their fertility goals. Here’s an overview of the services we provide:
Sexual Health Assessments:
Treatment for Sexual Dysfunction:
Fertility Evaluation and Testing:
Fertility Counseling and Education:
Hormonal Therapy:
Lifestyle Modification:
At HealthZone MD Family and Sports Medicine Wellness Center, we are committed to helping individuals and couples achieve optimal sexual health and fertility through personalized, evidence-based care. Whether you’re seeking treatment for sexual dysfunction, undergoing fertility evaluation and treatment, or simply looking to optimize your reproductive health, our experienced team is here to support you every step of the way. Schedule a consultation with us today to learn more about our sexual health and fertility support services and take the first step toward achieving your reproductive goals.
At HealthZone MD Family and Sports Medicine Wellness Center, we believe that regular exercise and physical activity are essential components of a healthy lifestyle. That’s why we offer comprehensive exercise and fitness programs designed to help you achieve your health and fitness goals, improve your overall well-being, and enhance your quality of life. Our exercise and fitness programs are tailored to meet the unique needs and preferences of individuals of all ages, fitness levels, and abilities. Here’s an overview of the services we provide:
Personalized Fitness Assessments:
Customized Exercise Prescription:
One-on-One Personal Training:
Group Fitness Classes:
Functional Movement Training:
Nutritional Counseling:
At HealthZone MD Family and Sports Medicine Wellness Center, our exercise and fitness programs are designed to empower you with the knowledge, skills, and support you need to lead an active and healthy lifestyle. Whether you’re new to exercise or a seasoned athlete, our experienced team is here to help you reach your full potential and live your best life. Schedule a consultation with us today to learn more about our exercise and fitness services and take the first step toward a healthier, happier you.
At HealthZone MD Family and Sports Medicine Wellness Center, we understand the profound impact that stress can have on your overall health and well-being. That’s why we offer comprehensive stress management and relaxation techniques to help you effectively cope with stress and achieve a greater sense of balance, tranquility, and inner peace. Our stress management program encompasses various evidence-based strategies and therapeutic approaches tailored to meet your unique needs and preferences. Here’s an overview of our stress management and relaxation services:
Mindfulness Meditation:
Relaxation Techniques:
Stress Reduction Strategies:
Lifestyle Counseling:
At HealthZone MD Family and Sports Medicine Wellness Center, our stress management and relaxation program is designed to empower you with the knowledge, skills, and support you need to effectively manage stress and cultivate a greater sense of well-being in your life. Whether you’re dealing with work-related stress, relationship issues, or other life challenges, we’re here to help you navigate your journey toward greater resilience, balance, and vitality. Schedule a consultation with our team today to learn more about our stress management services and start your path to a healthier, happier life.
At HealthZone MD Family and Sports Medicine Wellness Center, our Infusion Therapy Center is dedicated to providing cutting-edge intravenous (IV) therapy solutions to optimize your health and well-being. We offer a wide range of infusion therapies administered by experienced healthcare professionals in a comfortable and nurturing environment. Here’s an overview of our infusion therapy services:
Myers Cocktail:
Illness Recovery Therapy:
Immunity Boost Therapy:
Hangover Relief Therapy:
Energy Boost Therapy:
Detoxification Therapy:
Customized Infusion Therapy:
At HealthZone MD Family and Sports Medicine Wellness Center, our Infusion Therapy Center is committed to delivering safe, effective, and personalized IV therapy solutions to help you achieve optimal health and vitality. Whether you’re seeking immune support, energy enhancement, detoxification, or symptom relief, our infusion therapies are designed to rejuvenate your body and elevate your well-being. Schedule a consultation with our healthcare team today to discover the benefits of infusion therapy and start your journey toward improved health and vitality.
At HealthZone MD Family and Sports Medicine Wellness Center, we recognize the profound impact that hormonal imbalance can have on your overall health and well-being. Hormones play a crucial role in regulating various bodily functions, including metabolism, mood, energy levels, sleep patterns, and reproductive health. When hormone levels become imbalanced, it can lead to a wide range of symptoms and health issues.
Our Hormonal Imbalance and Hormonal Therapy program is designed to address hormonal imbalances and optimize hormone levels to help you feel your best. Here’s how we approach hormonal imbalance and the therapies we offer:
Comprehensive Assessment:
Personalized Treatment Plan:
Hormone Replacement Therapy (HRT):
Ongoing Monitoring and Support:
Whether you’re experiencing symptoms of menopause, andropause, thyroid dysfunction, adrenal fatigue, or other hormonal imbalances, HealthZone MD Family and Sports Medicine Wellness Center’s Hormonal Imbalance and Hormonal Therapy program can help. Our compassionate healthcare providers are committed to providing personalized care and empowering you to reclaim your health and vitality. Schedule a consultation with us to learn more about our hormonal therapy options and how we can support you on your journey to hormonal balance and well-being.
At HealthZone MD Family and Sports Medicine Wellness Center, we understand that looking and feeling your best is an essential component of overall well-being. Our Anti-aging, Botox, and cosmetic treatments are designed to help you achieve a youthful appearance and boost your confidence. Here’s an overview of the services we offer in this area:
Botox Injections:
Dermal Fillers:
Whether you’re looking to minimize the signs of aging, enhance your facial features, or rejuvenate your skin, HealthZone MD Family and Sports Medicine Wellness Center’s Anti-aging, Botox, and cosmetic treatments can help you achieve natural-looking, beautiful results that leave you feeling confident and rejuvenated. Schedule a consultation with our experienced healthcare providers to explore your options and discover how we can help you look and feel your best at any age.
At HealthZone MD Family and Sports Medicine Wellness Center, nutritional guidance and counseling play a pivotal role in promoting overall health, wellness, and disease prevention. The center’s approach to nutritional guidance encompasses personalized assessments, evidence-based recommendations, and ongoing support to empower individuals to make informed choices about their diet and lifestyle. Here’s an overview of the nutritional guidance and counseling services offered:
Personalized Nutritional Assessments:
Evidence-Based Recommendations:
Education and Counseling:
Ongoing Support and Monitoring:
Overall, HealthZone MD Family and Sports Medicine Wellness Center’s nutritional guidance and counseling services are designed to empower individuals to take control of their health through informed dietary choices, personalized support, and evidence-based strategies for long-term wellness. By addressing nutritional needs comprehensively, the center helps individuals optimize their health, prevent chronic diseases, and achieve their wellness goals.
HealthZone MD offers personalized weight management programs tailored to individual needs. This includes dietary counseling, exercise plans, and behavioral interventions to help clients achieve and maintain a healthy weight. The focus is on sustainable lifestyle changes rather than quick fixes, promoting long-term success in weight management and obesity prevention. Our providers also employ prescription medications such as Semaglutide and other FDA approved weightloss prescriptions including vitamins and Supplements that have shown promising results for weight loss and are increasingly being used in clinical settings. Semaglutide belong to a class of drugs known as glucagon-like peptide-1 receptor agonists (GLP-1 RAs) which work by mimicking the action of natural GLP-1 hormones in the body. Clinical trials have demonstrated that semaglutide can lead to significant weight loss in individuals with obesity or overweight, even in the absence of diabetes.
Semaglutide works by reducing appetite, increasing feelings of fullness, and slowing gastric emptying, which can result in reduced calorie intake and weight loss. At HealthZone MD Family and Sports Medicine Wellness Center, semaglutide and other weightloss medication may be prescribed as part of a comprehensive weight loss program for individuals who have struggled to lose weight through diet and exercise alone. It is typically administered via subcutaneous injection once weekly. It’s important to note that semaglutide is a prescription medication and should only be used under the supervision of a qualified healthcare provider. Before prescribing these medications, healthcare providers at HealthZone MD Family and Sports Medicine Wellness Center will conduct a thorough evaluation to assess each individual’s medical history, current health status, and weight loss goals. They will also provide guidance on proper medication use, potential side effects, and lifestyle modifications to optimize weight loss outcomes.
Personalized Health Assessments: Our Wellness Program begins with a thorough health assessment conducted by our experienced healthcare providers. During this assessment, we gather information about each individual’s medical history, lifestyle habits, and health goals. Based on this assessment, we develop personalized wellness plans tailored to address specific needs and objectives. Preventive Care and Screenings: We emphasize the importance of preventive care and offer a wide range of screenings and health assessments to detect potential health risks early. From routine blood tests and cholesterol screenings to cancer screenings and immunizations, we help individuals stay proactive about their health and identify any underlying issues before they escalate.
Nutrition and Exercise Guidance: Good nutrition and regular exercise are essential components of a healthy lifestyle. Our Wellness Program includes personalized nutrition counseling and exercise guidance to help individuals make informed choices about their diet and physical activity. We offer practical tips, meal plans, and exercise routines tailored to each person’s unique needs and preferences. Stress Management and Mental Health Support: Mental health is equally important as physical health. We provide resources and support for stress management, anxiety, depression, and other mental health concerns. Our team offers counseling, relaxation techniques, mindfulness practices, and referrals to mental health specialists as needed to support emotional well-being.
Chronic Disease Management: For individuals with chronic conditions such as diabetes, hypertension, or heart disease, our Wellness Program offers comprehensive management and support. We work closely with patients to develop personalized treatment plans, monitor disease progression, and optimize medication management to achieve optimal health outcomes. Lifestyle Modification Strategies: Our Wellness Program focuses on empowering individuals to make sustainable lifestyle changes that promote long-term health and wellness. We provide education and support for smoking cessation, weight management, sleep hygiene, and other lifestyle modifications to help individuals adopt healthier habits and reduce disease risk.
Community Engagement and Support: We believe in the power of community and offer opportunities for individuals to connect with others who share similar health goals and interests. Through group classes, workshops, support groups, and community events, we foster a supportive environment where individuals can learn, grow, and motivate each other on their wellness journey. HealthZone MD Family and Sports Medicine Wellness Center’s Wellness Program is a comprehensive and holistic approach to promoting health and wellness for individuals of all ages and backgrounds. By addressing physical, mental, and emotional well-being through personalized care plans, preventive screenings, nutrition and exercise guidance, stress management, chronic disease management, lifestyle modifications, and community support, we empower individuals to live healthier, happier lives. Our dedicated team of healthcare professionals is committed to partnering with each individual to achieve their wellness goals and thrive in all aspects of life.
We firmly believe that the internet should be available and accessible to anyone, and are committed to providing a website that is accessible to the widest possible audience, regardless of circumstance and ability.
To fulfill this, we aim to adhere as strictly as possible to the World Wide Web Consortium’s (W3C) Web Content Accessibility Guidelines 2.1 (WCAG 2.1) at the AA level. These guidelines explain how to make web content accessible to people with a wide array of disabilities. Complying with those guidelines helps us ensure that the website is accessible to all people: blind people, people with motor impairments, visual impairment, cognitive disabilities, and more.
This website utilizes various technologies that are meant to make it as accessible as possible at all times. We utilize an accessibility interface that allows persons with specific disabilities to adjust the website’s UI (user interface) and design it to their personal needs.
Additionally, the website utilizes an AI-based application that runs in the background and optimizes its accessibility level constantly. This application remediates the website’s HTML, adapts Its functionality and behavior for screen-readers used by the blind users, and for keyboard functions used by individuals with motor impairments.
If you’ve found a malfunction or have ideas for improvement, we’ll be happy to hear from you. You can reach out to the website’s operators by using the following email
Our website implements the ARIA attributes (Accessible Rich Internet Applications) technique, alongside various different behavioral changes, to ensure blind users visiting with screen-readers are able to read, comprehend, and enjoy the website’s functions. As soon as a user with a screen-reader enters your site, they immediately receive a prompt to enter the Screen-Reader Profile so they can browse and operate your site effectively. Here’s how our website covers some of the most important screen-reader requirements, alongside console screenshots of code examples:
Screen-reader optimization: we run a background process that learns the website’s components from top to bottom, to ensure ongoing compliance even when updating the website. In this process, we provide screen-readers with meaningful data using the ARIA set of attributes. For example, we provide accurate form labels; descriptions for actionable icons (social media icons, search icons, cart icons, etc.); validation guidance for form inputs; element roles such as buttons, menus, modal dialogues (popups), and others. Additionally, the background process scans all of the website’s images and provides an accurate and meaningful image-object-recognition-based description as an ALT (alternate text) tag for images that are not described. It will also extract texts that are embedded within the image, using an OCR (optical character recognition) technology. To turn on screen-reader adjustments at any time, users need only to press the Alt+1 keyboard combination. Screen-reader users also get automatic announcements to turn the Screen-reader mode on as soon as they enter the website.
These adjustments are compatible with all popular screen readers, including JAWS and NVDA.
Keyboard navigation optimization: The background process also adjusts the website’s HTML, and adds various behaviors using JavaScript code to make the website operable by the keyboard. This includes the ability to navigate the website using the Tab and Shift+Tab keys, operate dropdowns with the arrow keys, close them with Esc, trigger buttons and links using the Enter key, navigate between radio and checkbox elements using the arrow keys, and fill them in with the Spacebar or Enter key.Additionally, keyboard users will find quick-navigation and content-skip menus, available at any time by clicking Alt+1, or as the first elements of the site while navigating with the keyboard. The background process also handles triggered popups by moving the keyboard focus towards them as soon as they appear, and not allow the focus drift outside of it.
Users can also use shortcuts such as “M” (menus), “H” (headings), “F” (forms), “B” (buttons), and “G” (graphics) to jump to specific elements.
We aim to support the widest array of browsers and assistive technologies as possible, so our users can choose the best fitting tools for them, with as few limitations as possible. Therefore, we have worked very hard to be able to support all major systems that comprise over 95% of the user market share including Google Chrome, Mozilla Firefox, Apple Safari, Opera and Microsoft Edge, JAWS and NVDA (screen readers), both for Windows and for MAC users.
Despite our very best efforts to allow anybody to adjust the website to their needs, there may still be pages or sections that are not fully accessible, are in the process of becoming accessible, or are lacking an adequate technological solution to make them accessible. Still, we are continually improving our accessibility, adding, updating and improving its options and features, and developing and adopting new technologies. All this is meant to reach the optimal level of accessibility, following technological advancements. For any assistance, please reach out to